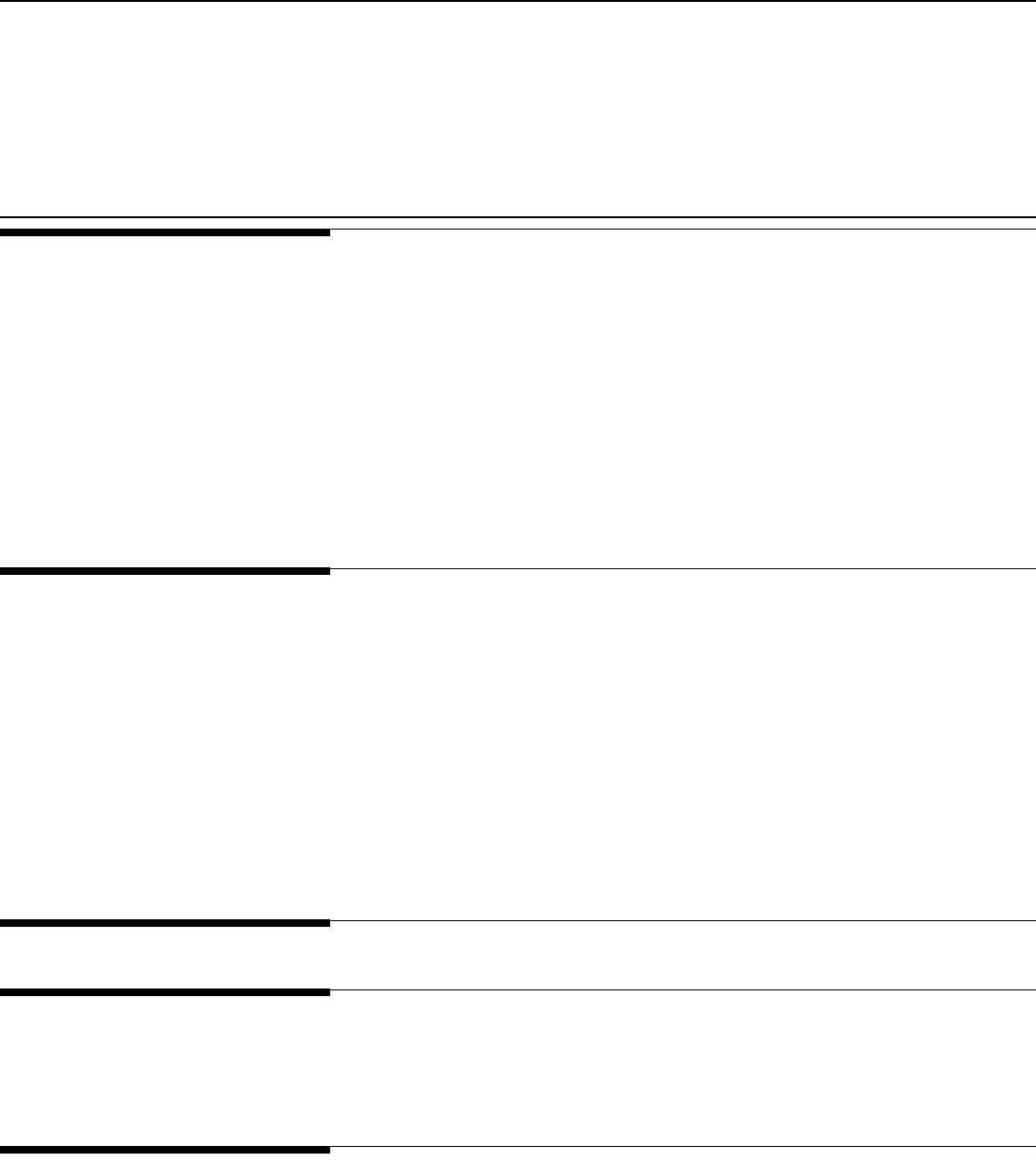
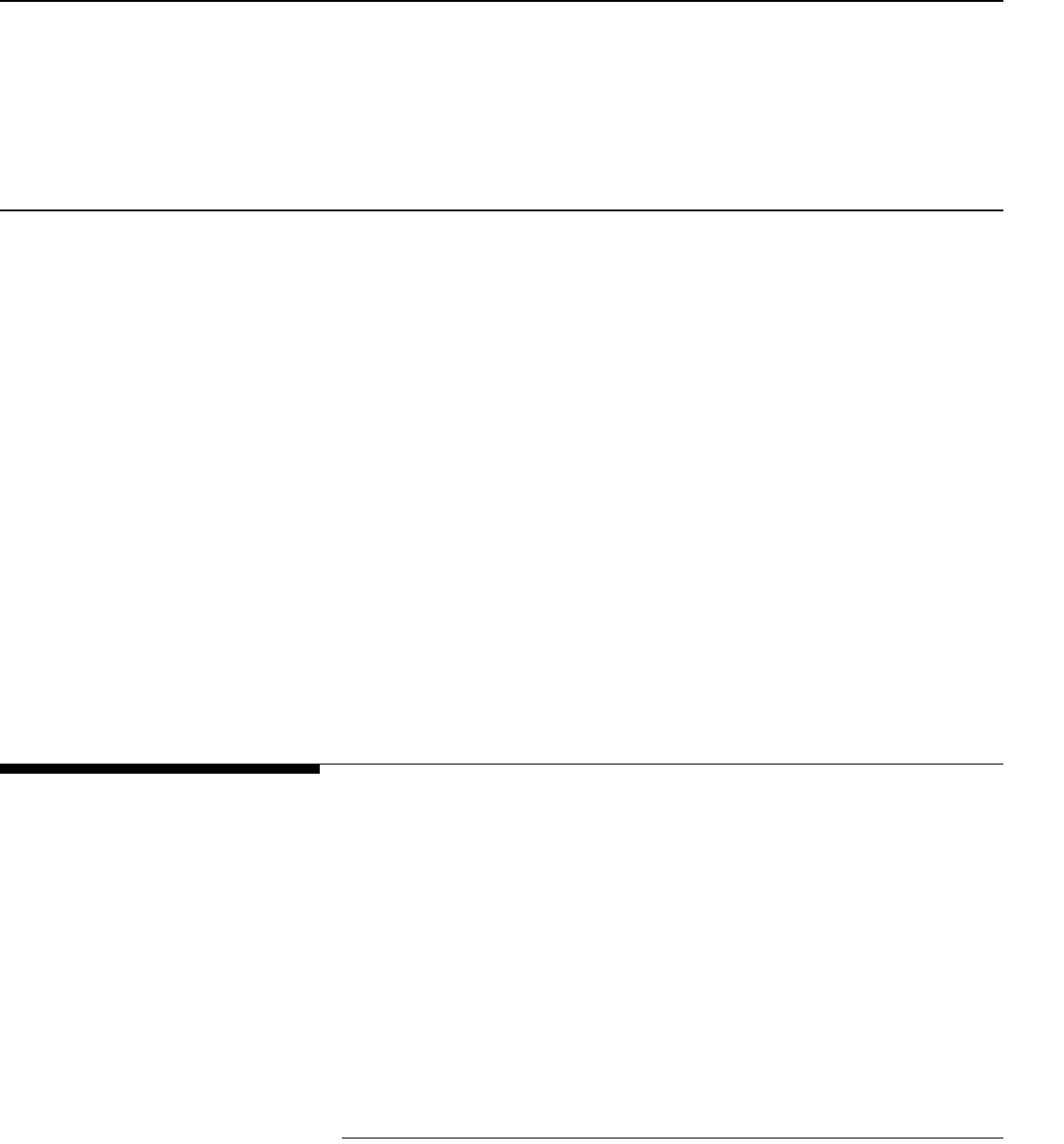
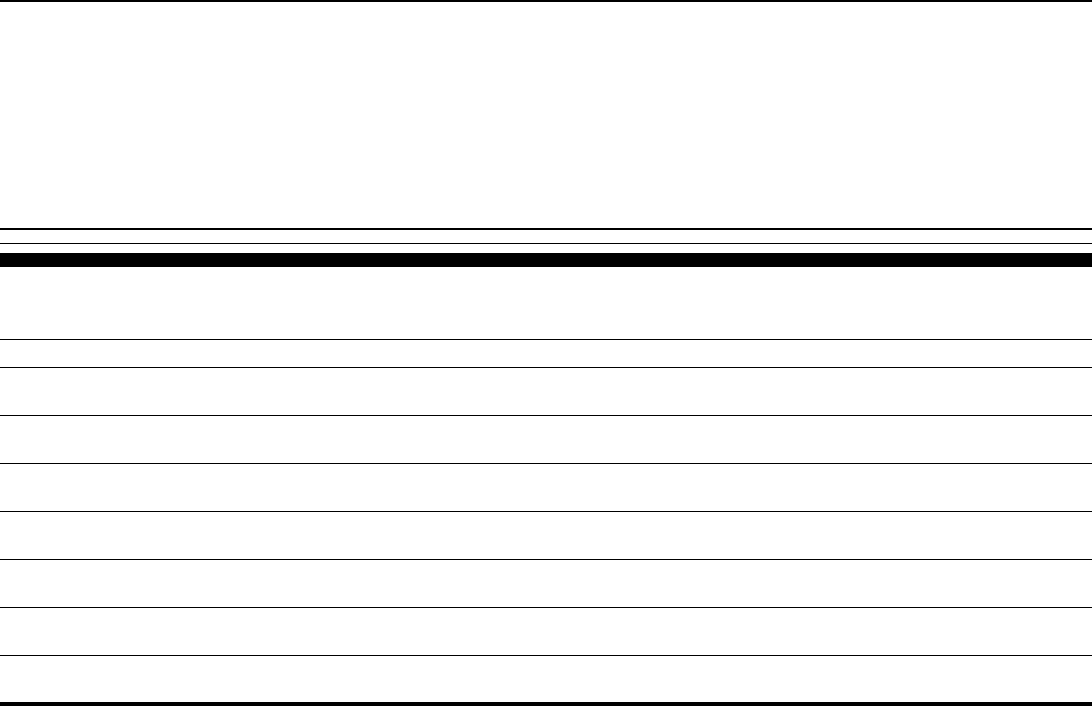
Since 1999, medical malpractice premium rates have increased dramatically
for physicians in some specialties in a number of states. However, among
larger insurers in the seven states GAO analyzed, both the premium rates
and the extent to which these rates have increased varied greatly (see
figure).
Multiple factors, including falling investment income and rising reinsurance
costs, have contributed to recent increases in premium rates in our sample
states. However, GAO found that losses on medical malpractice claims—
which make up the largest part of insurers’ costs—appear to be the primary
driver of rate increases in the long run. And while losses for the entire
industry have shown a persistent upward trend, insurers’ loss experiences
have varied dramatically across our sample states, resulting in wide
v
ariations in premium rates. In addition, factors other than losses can affect
p
remium rates in the short run, exacerbating cycles within the medical
malpractice market. For example, high investment income or adjustments
to account for lower than expected losses may legitimately permit insurers
to price insurance below the expected cost of paying claims. However,
because of the long lag between collecting premiums and paying claims,
underlying losses may be increasing while insurers are holding premium
rates down, requiring large premium rate hikes when the increasing trend in
losses is recognized. While these factors may explain some events in the
medical malpractice market, GAO could not fully analyze the composition
and causes of losses at the insurer level owing to a lack of comprehensive
data.
GAO’s analysis also showed that the medical malpractice market has
changed considerably since previous hard markets. Physician-owned and/or
operated insurers now cover around 60 percent of the market, self-insurance
has become more widespread, and states have passed laws designed to
reduce premium rates. As a result, it is not clear how premium rates might
behave during future soft or hard markets.
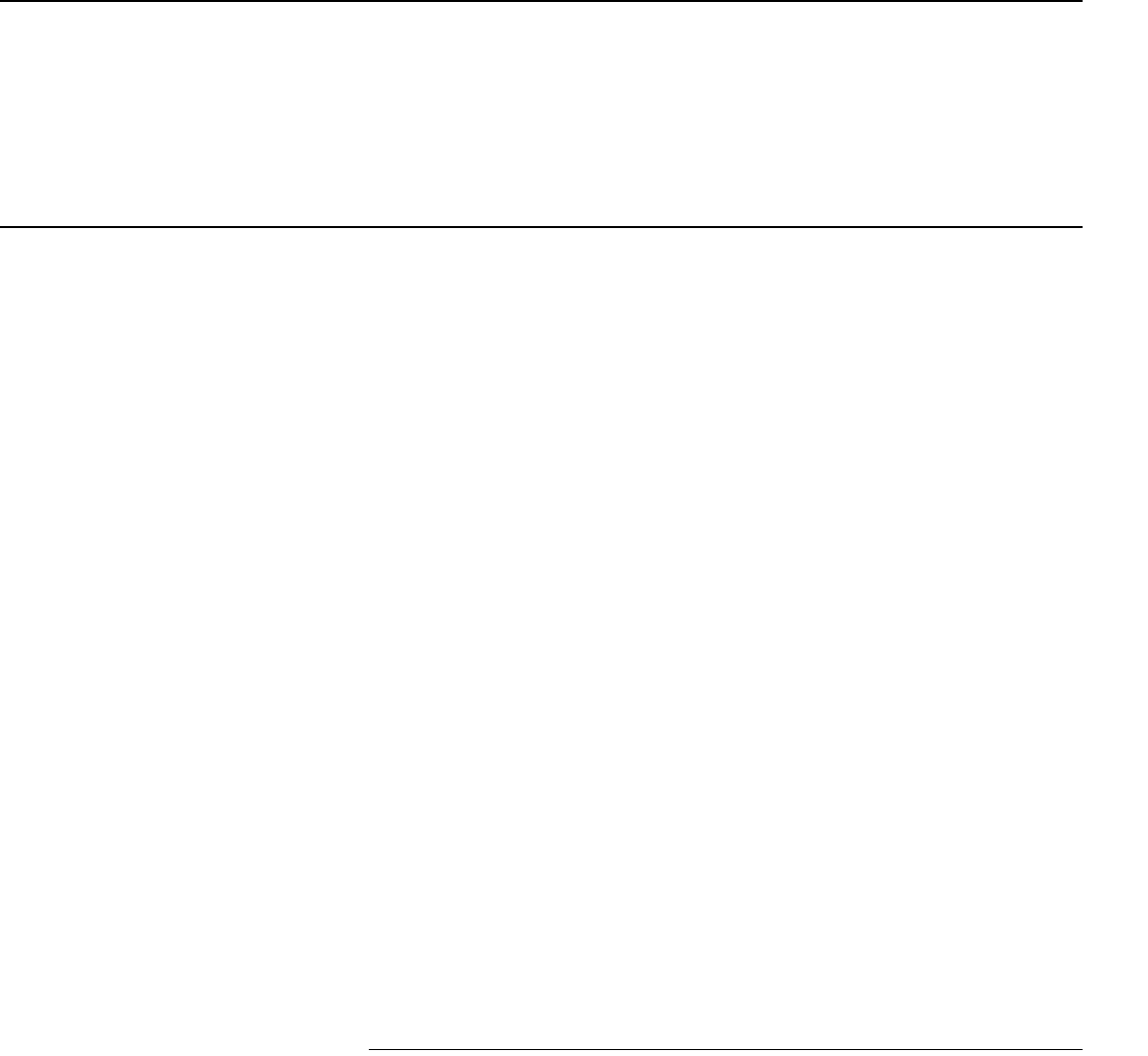
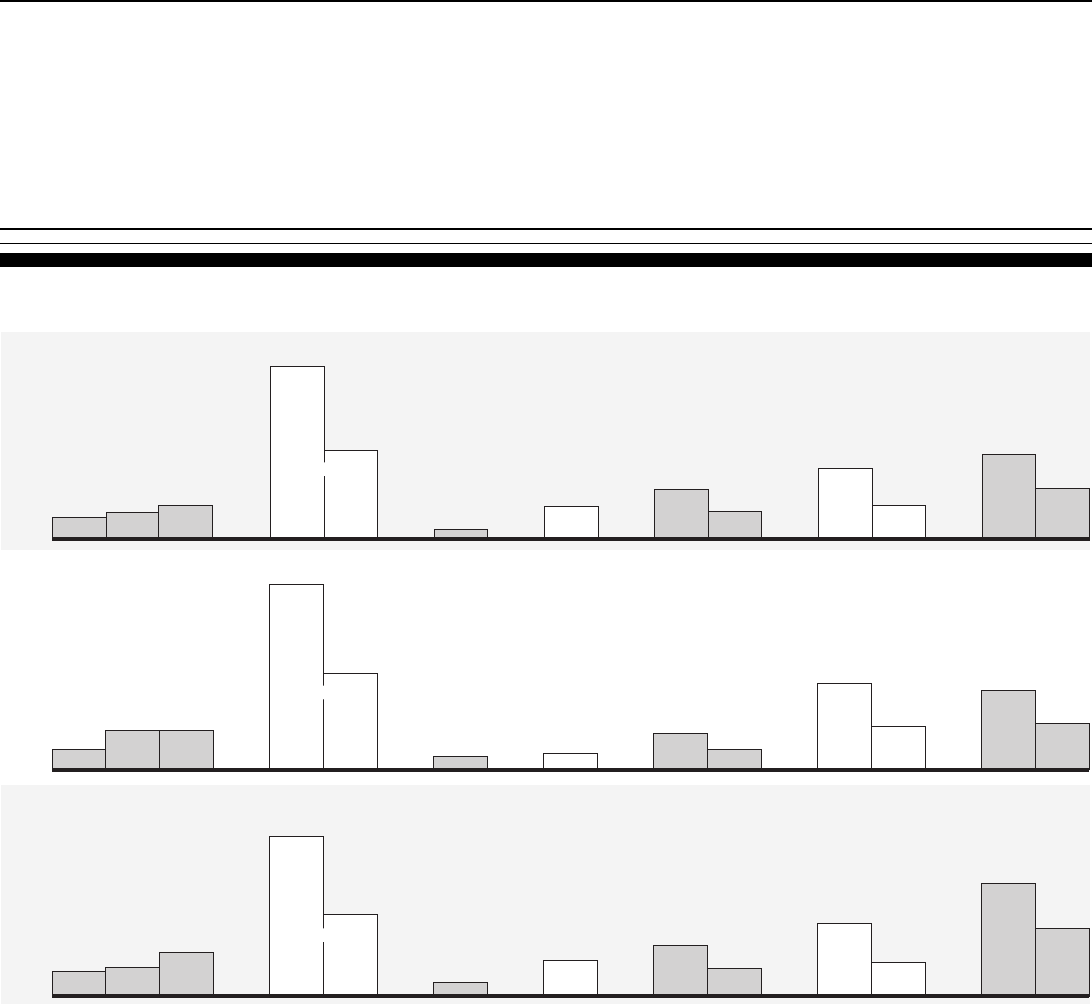
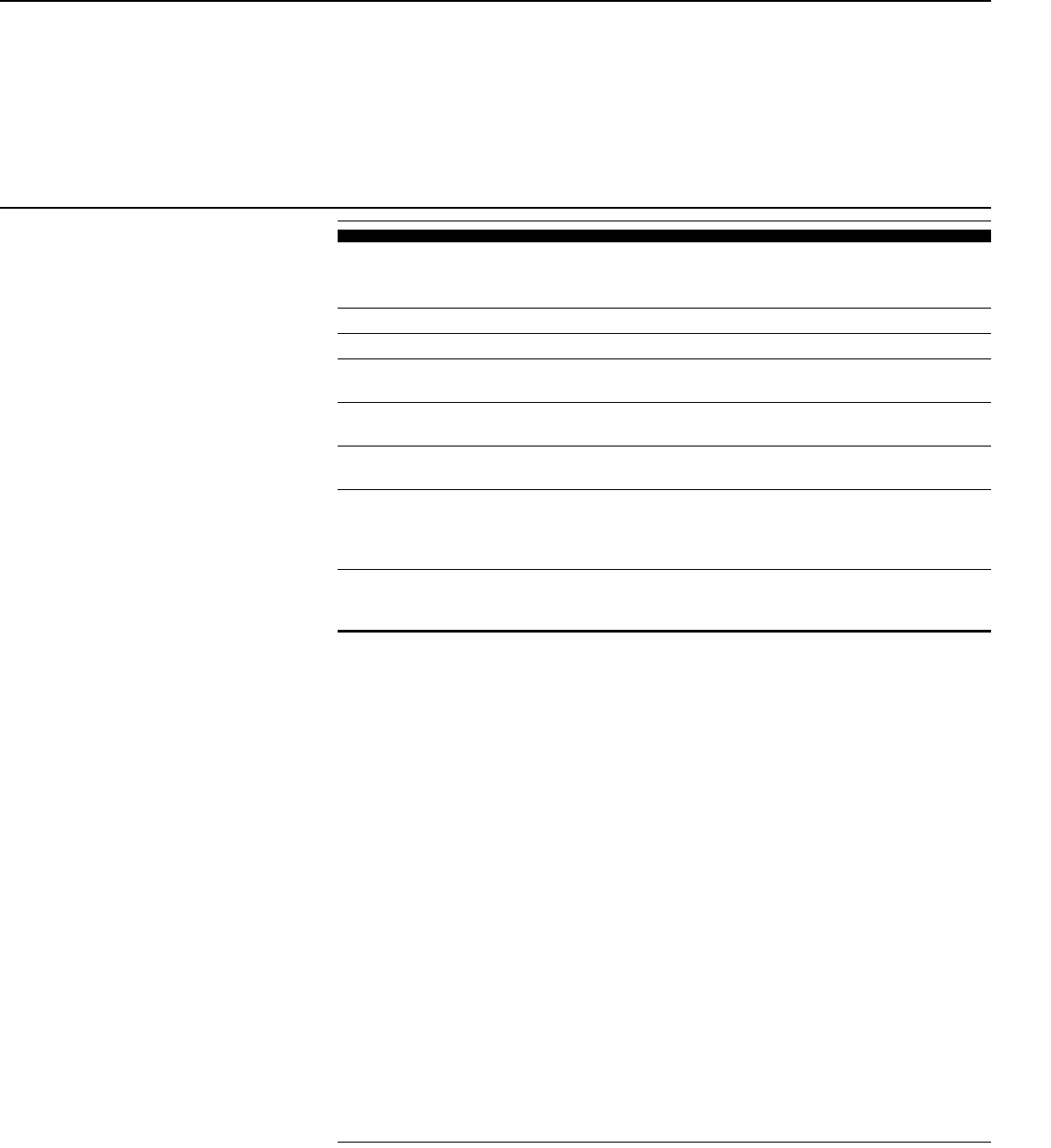
Medical Malpractice Premium Base Rates for Obstetricians and Gynecologists Quoted by
Larger Insurers in 1998 and 2002 in the Seven States GAO Visited (Dollars in Thousands)
Source: GAO analysis of annual surveys by the Medical Liability Monitor.
PMSLIC
(Philadelphia,
Pennsylvania)
TMLT
(El Paso,
Texas)
MIEC
(Clark
County,
Nevada)
MMIC
(Minnesota)
MACM
(Mississippi)
FPIC
(Dade
County,
Florida)
FPIC
(rest of
Florida)
Doctor's
Company
(northern
California)
0
50
100
150
200
250
34
31
140
201
76
103
18
17
37
45
95
142
29
64
58
92
1998 2002
Over the past several years, large
increases in medical malpractice
insurance premium rates have
raised concerns that physicians will
no longer be able to afford
malpractice insurance and will be
forced to curtail or discontinue
providing certain services.
Additionally, a lack of profitability
has led some large insurers to stop
selling medical malpractice
insurance, furthering concerns that
physicians will not be able to
obtain coverage. To help Congress
better understand the reasons
behind the rate increases, GAO
undertook a study to (1) describe
the extent of the increases in
medical malpractice insurance
rates, (2) analyze the factors that
contributed to those increases, and
(3) identify changes in the medical
malpractice insurance market that
might make this period of rising
premium rates different from
previous such periods.
GAO is not recommending
executive action. However, to
further the understanding of
conditions in current and future
medical malpractice markets,
Congress may wish to consider
encouraging the National
Association of Insurance
Commissioners and state insurance
regulators to identify and collect
additional, mutually beneficial data
necessary for evaluating the
medical malpractice insurance
market.
www.gao.gov/cgi-bin/getrpt?GAO-03-702.
To view the full product, including the scope
and methodology, click on the link above.
For more information, contact Richard J.
Hillman at (202) 512-8678 or
Highlights of GAO-03-702, a report to
congressional requesters
June 2003
MEDICAL MALPRACTICE INSURANCE
Multiple Factors Have Contributed to
Increased Premium Rates
Page i GAO-03-702 Medical Malpractice Insurance
Contents
Letter 1
Results in Brief 3
Background 6
Both the Extent of Increases in Medical Malpractice Premium Rates
and the Rates Themselves Varied across Specialties and States 9
Multiple Factors Have Contributed to the Increases in Medical
Malpractice Premium Rates 15
The Medical Malpractice Insurance Market Has Changed since
Previous Hard Markets 37
Conclusions 43
Matter for Congressional Consideration 46
NAIC Comments and Our Evaluation 46
Appendixes
Appendix I: Scope and Methodology 49
Appendix II: Legal Summary 51
Appendix III: State Summaries 55
Market Description 55
Insurer Characteristics and Market Share 56
Rate Regulation 56
State Tort Laws 57
Appendix IV: GAO Contacts and Staff Acknowledgments 66
GAO Contacts 66
Acknowledgments 66
Related GAO Products
67
Tables
Table 1: Annual Yields for Selected Bonds, 1995–2002, and Average
Return on Investment Assets, 1997–2002, for the 15 Largest
Writers of Medical Malpractice Insurance in 2001 25
Table 2: Hypothetical Example of How Premium Rates Change
When the Return on Investments Falls 27
Figures
Figure 1: Premium Base Rates of the Largest Insurers in Seven
Selected States for Three Medical Specialties,
1992–2002 11
Contents
Page ii GAO-03-702 Medical Malpractice Insurance
Figure 2: Percentage Changes in Premium Base Rates of the
Largest Medical Malpractice Insurers in Seven Selected
States for Three Medical Specialties, 1999–2002 12
Figure 3: 2002 Medical Malpractice Insurance Premium Base Rates
of the Largest Insurers in Seven Selected States for Three
Medical Specialties 14
Figure 4: Inflation-Adjusted Paid and Incurred Losses for the
National Medical Malpractice Insurance Market, 1975–
2001 (Using the CPI, in 2001 Dollars) 17
Figure 5: Inflation-Adjusted Aggregate Paid Losses for Medical
Malpractice Insurers in Seven Selected States, 1975-2001
(Using the CPI, in 2001 Dollars) 19
Figure 6: Inflation-Adjusted Aggregate Incurred Losses for Medical
Malpractice Insurers in Seven Selected States, 1975-2001
(Using the CPI, in 2001 Dollars) 21
Figure 7: Net Profit or Loss as a Percentage of Net Worth for
Medical Malpractice Insurance Companies Nationwide,
1990–2001 29
Figure 8: Aggregate Incurred Losses as a Percentage of Premiums
Earned for Medical Malpractice Insurers in Seven
Selected States, 1975–2001 30
Figure 9: Incurred Losses as a Percentage of Premium Income for
Medical Malpractice Insurers and Property-Casualty
Insurers Nationwide, 1976–2001 34
Figure 10: California 59
Figure 11: Florida 60
Figure 12: Minnesota 61
Figure 13: Mississippi 62
Figure 14: Nevada 63
Figure 15: Pennsylvania 64
Figure 16: Texas 65

Contents
Page iii GAO-03-702 Medical Malpractice Insurance
Abbreviations
AMA American Medical Association
CAP/MPT Cooperative of American Physicians/
Mutual Protection Trust
CDI California Department of Insurance
CPI Consumer Price Index
DOI Department of Insurance
FMA Florida Medical Association
FPIC First Professionals Insurance Company
JUA Joint Underwriting Association
MACM Medical Assurance Company of Mississippi
MIEC Medical Insurance Exchange of California
MIIX Medical Inter-Insurance Exchange
MLM Medical Liability Monitor
MMIC Midwest Medical Insurance Company
NAIC National Association of Insurance Commissioners
NMIC Nevada Mutual Insurance Company
NSCL National Conference of State Legislatures
PIAA Physician Insurers Association of America
PID Pennsylvania Insurance Department
PMSLIC Pennsylvania Medical Society Liability Insurance
Company
SCPIE Southern California Physicians Insurance Exchange
TMA Texas Medical Association
TMLT Texas Medical Liability Trust
This is a work of the U.S. government and is not subject to copyright protection in the
United States. It may be reproduced and distributed in its entirety without further
permission from GAO. However, because this work may contain copyrighted images or
other material, permission from the copyright holder may be necessary if you wish to
reproduce this material separately.
Page 1 GAO-03-702 Medical Malpractice Insurance
United States General Accounting Office
Washington, D.C. 20548
Page 1 GAO-03-702 Medical Malpractice Insurance
A
June 27, 2003 Letter
Congressional Requesters
Since the late 1990s, premium rates for medical malpractice insurance have
increased dramatically for physicians in certain specialties and states.
1
These increases have raised concerns that many physicians will no longer
be able to afford malpractice insurance and may be forced to curtail or
discontinue providing services. These concerns have been heightened as
some large insurers, faced with declining profits, have either stopped
selling medical malpractice insurance or reduced their operations in a
number of states. But disagreement exists over the causes of increased
premium rates and what, if anything, should be done in response to the
current situation. For example, some have argued for tort reform as a
means of lowering certain awards in medical malpractice lawsuits and
advocate legislative changes at the state level designed to place a cap on
such awards. Others have argued for medical reforms as a means of
reducing the incidence of medical malpractice or for insurance reforms as
a way to moderate premium rate increases.
In response to these concerns, you asked us to determine the reasons
behind the recent increases in some medical malpractice insurance rates.
2
Our specific objectives were to (1) describe the extent of the increases in
medical malpractice insurance rates, (2) analyze the factors that have
contributed to the increases, and (3) identify changes in the medical
malpractice insurance market that may make the current period of rising
premium rates different from earlier periods of rate hikes. We will also
1
Medical malpractice lawsuits are generally based on tort law, which includes both statutes
and court decisions. A tort is a wrongful act or omission by an individual that causes harm
to another individual. Typically, a malpractice tort would be based on the claim that the
health care provider was negligent, had failed to meet the acceptable standard of care owed
to the patient, and thus had caused injury to the patient.
2
Some health care provider associations and others have expressed concern over medical
malpractice insurance premium rates for nursing homes and hospitals, but this topic is
outside the scope of our report.
Page 2 GAO-03-702 Medical Malpractice Insurance
issue a related report that describes the effect of rising malpractice
premiums on access to health care and related issues.
3
Recognizing that the medical malpractice market can vary considerably
across states, as part of our review we judgmentally selected a sample of
seven states—California, Florida, Minnesota, Mississippi, Nevada,
Pennsylvania, and Texas—in order to conduct a more in depth review in
each of those states. Our sample contains a mix of states based on the
following characteristics: extent of any recent increases in premium rates,
status as a “crisis state” according to the American Medical Association,
presence of caps on noneconomic damages, state population, and
aggregate loss ratios for medical malpractice insurers within the state.
Except where noted otherwise, our analyses were limited to these states.
Within each state, we spoke to one or both of the two largest and currently
active medical malpractice insurers,
4
the state insurance regulator, and the
state association of trial attorneys. In six states, we spoke to the state
medical association, and in five states, we spoke to the state hospital
association. To examine the extent of increases in medical malpractice
insurance rates in our sample states, we reviewed annual survey data
collected by a private company.
5
To analyze the factors contributing to the
premium rate increases in our sample states as well as nationally, we
reviewed data provided by medical malpractice insurers to state insurance
regulators, the National Association of Insurance Commissioners (NAIC),
6
3
For other related GAO products, see the list at the end of this report.
4
We determined the largest insurers in 2002 based on premiums written for calendar year
2001.
5
The Medical Liability Monitor annually surveys providers of medical malpractice
insurance to obtain their premium base rates for three different specialties: internal
medicine, general surgery, and obstetrics/gynecology.
6
NAIC is a voluntary association of the heads of each state insurance department, the
District of Columbia, and four U.S. territories. NAIC assists state insurance regulators by
providing guidance, model (or recommended) laws and guidelines, and information-sharing
tools.
Page 3 GAO-03-702 Medical Malpractice Insurance
and A.M. Best
7
on insurers within our sample states as well as the 15 largest
writers of medical malpractice insurance nationally in 2001 (whose
combined market share nationally was approximately 64.3 percent). We
also spoke with officials from professional actuarial and insurance
organizations and national trial attorney and medical associations and
reviewed their testimonies before Congress. In addition, we analyzed data
on medical malpractice claims collected by insurers, state regulators, and
others in our sample states as well as nationally.
To analyze how the national medical malpractice insurance market has
changed since previous periods of rising premium rates, we reviewed
studies published by NAIC, reviewed state insurance regulations and tort
laws, and spoke to the insurers and state insurance departments in our
sample states. We also spoke to officials from national professional
actuarial, legal, and insurance organizations. Appendix I contains a more
detailed description of our methodology.
Results in Brief
Since 1999, medical malpractice premium rates
for physicians in some
states have increased dramatically. Among the seven states that we
analyzed, we found that both the extent of the increases and the premium
levels varied greatly not only from state to state but across medical
specialties and even among areas within states. For example, the largest
writer of medical malpractice insurance in Florida increased premium
rates for general surgeons in Dade County by approximately 75 percent
from 1999 to 2002, while the largest insurer in Minnesota increased
premium rates for the same specialty by about 2 percent over the same
period. The resulting 2002 premium rate quoted by the insurer in Florida
was $174,300 a year, more than 17 times the $10,140 premium rate quoted
by the insurer in Minnesota. In addition, the Florida insurer quoted a rate
for general surgeons outside Dade County of $89,000 a year for the same
coverage, approximately 51 percent of the rate it quoted inside Dade
County.
7
A.M. Best is a rating agency that provides current or prospective investors, creditors, and
policyholders with independent analyses of insurance companies’ overall financial strength,
creditworthiness, ability to pay claims, and company activities.
Page 4 GAO-03-702 Medical Malpractice Insurance
Multiple factors have contributed to the recent increases in medical
malpractice premium rates in the seven states we analyzed. First, since
1998 insurers’ losses on medical malpractice claims have increased rapidly
in some states. For example, in Mississippi the amount insurers paid
annually on medical malpractice claims, or paid losses,
8
increased by
approximately 142 percent from 1998 to 2001 after adjusting for inflation.
9
We found that the increased losses appeared to be the greatest contributor
to increased premium rates, but a lack of comprehensive data at the
national and state levels on insurers’ medical malpractice claims and the
associated losses prevented us from fully analyzing the composition and
causes of those losses. For example, data that would have allowed us to
analyze claim severity at the insurer level on a state-by-state basis or
determine how losses were broken down between economic and
noneconomic damages were unavailable. Second, from 1998 through 2001
medical malpractice insurers experienced decreases in their investment
income
10
as interest rates fell on the bonds that generally make up around
80 percent of these insurers’ investment portfolios. While almost no
medical malpractice insurers experienced net losses on their investment
portfolios over this period, a decrease in investment income meant that
income from insurance premiums had to cover a larger share of insurers’
costs. Third, during the 1990s insurers competed vigorously for medical
malpractice business, and several factors, including high investment
returns, permitted them to offer prices that in hindsight, for some insurers,
did not completely cover their ultimate losses on that business. As a result
of this, some companies became insolvent or voluntarily left the market,
reducing the downward competitive pressure on premium rates that had
existed through the 1990s. Fourth, beginning in 2001 reinsurance rates for
medical malpractice insurers also increased more rapidly than they had in
8
Paid losses are the cash payments insurers made in a given period, such as a calendar year,
on claims reported during both the current and previous years. Incurred losses include the
insurer’s expected costs for claims reported in that year and adjustments to the expected
costs for claims reported in earlier years. In Mississippi, insurers’ incurred losses increased
approximately 197.5 percent from 1998 to 2001, after adjusting for inflation.
9
We adjusted for inflation using the consumer price index (CPI). The CPI is a measure of the
average change over time in the prices consumers pay for a basket of goods and services.
This report uses the CPI-U, which is meant to reflect the spending patterns of urban
consumers and covers about 87 percent of the total U.S. population.
10
In general, state insurance regulators require insurers to reduce their requested premium
rates in line with expected investment income. That is, the higher the expected income from
investments, the more premium rates must be reduced.
Page 5 GAO-03-702 Medical Malpractice Insurance
the past, raising insurers’ overall costs.
11
In combination, all of these
factors contribute to the movement of the medical malpractice insurance
market through cycles of hard and soft markets--similar to those
experienced by the property-casualty insurance market as a whole--during
which premium rates fluctuate.
12
Cycles in the medical malpractice market
tend to be more extreme than in other insurance markets because of the
longer period of time required to resolve medical malpractice claims, and
factors such as changes in investment income and reduced competition can
exacerbate the fluctuations.
While the medical malpractice insurance market as a whole had
experienced periods of rapidly increasing premium rates during previous
hard markets in the mid-1970s and mid-1980s, the market has changed
considerably since then. These changes are largely the result of actions
insurers, health care providers, and states have taken to address increasing
premium rates. Beginning in the 1970s and 1980s, insurers began selling
“claims-made” rather than “occurrence-based” policies,
13
enabling insurers
to better predict losses for a particular year. Also in the 1970s, physicians,
facing increasing premium rates and the departure of some insurers, began
to form mutual nonprofit insurance companies. Such companies, which
may have some cost and other advantages over commercial insurers, now
comprise a significant portion of the medical malpractice insurance
market. More recently, an increasing number of large hospitals and groups
of hospitals or physicians have left the traditional commercial insurance
market and begun to insure themselves in a variety of ways—for example,
by self-insuring. While such arrangements can save money on
administrative costs, hospitals and physicians insured through these
arrangements assume greater financial responsibility for malpractice
claims than they would under traditional insurance arrangements and thus
may face a greater risk of insolvency. Finally, since periods of increasing
11
Reinsurance is insurance for insurance companies, which insurance companies routinely
use as a way to spread the risk associated with their insurance policies.
12
Some industry officials have characterized hard markets as periods of rapidly rising
premium rates, tightened underwriting standards, narrowed coverage, and the withdrawal
of insurers from certain markets. Soft markets are characterized by relatively flat or slow-
rising premium rates, less stringent underwriting standards, expanded coverage and strong
competition among insurers.
13
Claims-made policies cover claims reported during the year in which the policy is in effect.
Occurrence-based policies cover claims arising out of events that occurred but may not
have been reported during the year in which the policy was in effect. Most policies sold
today are claims-made policies.
Page 6 GAO-03-702 Medical Malpractice Insurance
premium rates during the mid-1970s and mid-1980s, all states passed at
least some laws designed to reduce medical malpractice premium rates.
Some of these laws are designed to decrease insurers’ losses on medical
malpractice claims, while others are designed to more tightly control the
premium rates insurers can charge. These changes make it difficult to
predict how medical malpractice premiums might behave during future
hard and soft markets.
This report includes a matter that Congress may want to consider as it
looks for ways to improve the ability of Congress, state insurance
regulators, and others to analyze the current and future medical
malpractice insurance markets. Specifically, Congress may want to
consider encouraging NAIC and state insurance regulators to identify and
collect additional data necessary to evaluate the frequency,
14
severity,
15
and
causes of losses on medical malpractice claims.
We received comments on a draft of this report from NAIC’s Director of
Research. The Director generally agreed with the report’s findings and
matters for congressional consideration, and provided technical comments
that we have incorporated as appropriate. The Director’s comments are
discussed in greater detail at the end of this letter.
Background
Nearly all health care providers, such as physicians and hospitals, purchase
insurance that covers expenses related to medical malpractice claims,
including payments to claimants and legal expenses. The most common
physician policies provide $1 million of coverage per incident and
$3 million of coverage per year. Today the primary sellers of physician
medical malpractice insurance are the physician-owned and/or operated
insurance companies that, according to the Physician Insurers Association
of America, insure approximately 60 percent of all physicians in private
practice in the United States. Other health care providers may obtain
coverage through commercial insurance companies, mutual coverage
arrangements, or state-run insurance programs, or may self-insure (take
responsibility for claims themselves). Most medical malpractice insurance
policies offer claims-made coverage, which covers claims reported during
14
Claim frequency is the number of claims per exposure unit, such as a single general
practitioner.
15
Claim severity is the average loss per claim.
Page 7 GAO-03-702 Medical Malpractice Insurance
the year in which the policy is in effect. A small and declining number of
policies offer occurrence coverage, which covers all claims arising out of
events that occurred during the year in which the policy was in effect.
Medical malpractice insurance operates much like other types of
insurance, with insurers collecting premiums from policyholders in
exchange for an agreement to defend and pay future claims within the
limits set by the policy. Insurers invest the premiums they collect and use
the income from those investments to reduce the amount of premium
income that would have been required otherwise. Claims against a
policyholder are recorded as expenses, or incurred losses, which are equal
to the amount paid on those claims as well as the insurer’s estimate of
future losses on those same claims. The liability associated with the
portion of these incurred losses that have not yet been paid by the insurer
is collectively known as the insurer’s loss reserve. In order to maintain
financial soundness, insurers must maintain assets in excess of total
liabilities—including loss reserves and reserves for premiums received but
not yet earned
16
—to make up what is known as the insurer’s surplus. State
insurance departments monitor insurers’ solvency by tracking, among
other measures, the ratio of total annual premiums to this surplus. Medical
malpractice insurers generally attempt to keep their surplus approximately
equal to their annual premium income.
Medical malpractice insurers establish premium base rates for particular
medical specialties within a state and sometimes for particular geographic
regions within a state. Insurers may also offer discounts or add surcharges
for the particular characteristics of policyholders, such as claim histories
or whether they participate in risk-management programs. The premium
rates are based on anticipated losses on claims and related expenses,
expected investment income, the need to build a surplus, and, for for-profit
insurers, the desire to earn a reasonable profit for shareholders. In most
states the insurance regulators have the authority to approve or deny
proposed changes to premium rates.
16
Insurers collect premiums in advance for coverage during a future period of time, and as
that period of time passes, those premiums are “earned.” Premiums related to periods of
time yet to pass are considered “unearned” and are a liability on the books of the insurer.
Page 8 GAO-03-702 Medical Malpractice Insurance
For several reasons, accurately predicting losses on medical malpractice
claims is difficult. First, according to a national insurer association we
spoke with, most medical malpractice claims take an average of more than
5 years to resolve, including discovering the malpractice, filing a claim,
determining (through settlement or trial) payment responsibilities, if any,
and paying the claim.
17
In addition, some claims may not be resolved for as
long as 8 to 10 years. As a result, insurers often must estimate costs years in
advance. Second, the range of potential losses is wide. Actuaries we spoke
with told us that individual claims with similar characteristics can result in
very different losses for the insurer, making it difficult to predict the
ultimate cost of any single claim. Third, the predictive value of historical
data is further limited by the often small pool of relevant policyholders. For
example, a relevant pool of policyholders would be physicians practicing a
particular specialty within a specific state and perhaps within a specific
geographic area within that state. In smaller states, and for some of the less
common but more risky specialties, this pool could be very small and
provide only a limited amount of data that could be used to estimate future
costs.
Medical malpractice insurance is regulated by state insurance departments
and subject to state laws. That is, insurers selling medical malpractice
insurance in a particular state are subject to that state’s regulations for
their operations within that state, and all claims within that state are
subject to that state’s tort laws. Insurance regulations can vary across
states, creating differences in the way insurance rates are regulated. For
example, one state insurance regulator we spoke with essentially let the
insurance market determine appropriate rates, while another had an
increased level of review, including approving specific company rates on a
case-by-case basis. NAIC assists state insurance regulators in developing
these regulations by providing guidance, model (or recommended) laws
and guidelines, and information-sharing tools.
In response to concerns over rising premium rates, physicians, medical
associations, and insurers have pushed for state and federal legislation that
would, among other things, limit the amount of damages paid out on
medical malpractice claims. A few states have passed legislation with such
limitations over the past several years, and federal legislation is pending.
On March 13, 2003, the House of Representatives passed the Help Efficient,
17
Estimates of some individual insurers we spoke with ranged from around 3 years to over
5 years.
Page 9 GAO-03-702 Medical Malpractice Insurance
Accessible Low-Cost, Timely Healthcare (HEALTH) Act of 2003, which
includes, among other things, a limit on certain types of damages in
medical malpractice claims. On March 12, 2003, a similar bill of the same
name was introduced in the Senate, but as of June 2003, no additional
action had been taken.
Both the Extent of
Increases in Medical
Malpractice Premium
Rates and the Rates
Themselves Varied
across Specialties and
States
Beginning in 1999 and 2000, medical malpractice insurers in our seven
sample states increased their premium rates
18
for the physician specialties
of general surgery, internal medicine, and obstetrics/gynecology faster than
they had since at least 1992. These specialties were the only ones for which
data were available, and 1992 was the earliest year for which we could
obtain comprehensive survey data.
19
However, both the extent of these
changes and the level of the premium rates insurers charged varied greatly
across medical specialties, states, and even areas within states. From 1999
through 2002, one large insurer raised rates more for internal medicine
than for general surgery, while another raised rates 12 times more for
general surgery than for internal medicine. Changes in premium base rates
among some of the largest insurers in each state ranged from a reduction of
about 9 percent for obstetricians and gynecologists insured by one
California company to an increase of almost 170 percent for doctors in the
18
In this report, premium rates are the base rates insurers submit to state regulators along
with a schedule of potential deductions or additions related to the particular characteristics
of policyholders. The actual premium rate insurers charge individual policyholders varies
from the base rate. We could not determine the extent to which the actual premium rates
charged varied from the base rates, but among some of the insurers we spoke with, the
actual premium rates ranged from about 50 to 100 percent of the base rates over the past
several years. Some market observers and participants also told us that the discounts have
decreased over the last several years.
19
All premium rate information in this report is based on survey data collected by the
Medical Liability Monitor, a newsletter that, among other things, publishes the results of its
annual surveys of the premium rates of medical malpractice insurers. Comprehensive
survey data was available for years 1992 to 2002. The surveys, which are sent to medical
malpractice insurers, request premium rates for each state or smaller region for a standard
amount of coverage in three specialties—internal medicine, general surgery, and
obstetrics/gynecology. The Medical Liability Monitor selected these in order to have data
representative of low-, medium-, and high-risk specialties. In the survey results for 1999
through 2002, all 50 states were represented in the rate information that companies
provided. The premium rates collected in the survey are base rates that do not reflect the
discounts or the additional amounts insurers charge, so actual premium rates can vary from
the premium rates given in the survey.
Page 10 GAO-03-702 Medical Malpractice Insurance
same specialty in one area of Pennsylvania.
20
At the same time, premium
rates for the same amount of coverage for the same medical specialty
varied by a factor of as much as 17 among states—that is, the rate in one
state was 17 times higher than the rate in a different state.
Premium Rates Have Grown
Rapidly since 1998 for
Certain Specialties in Some
States
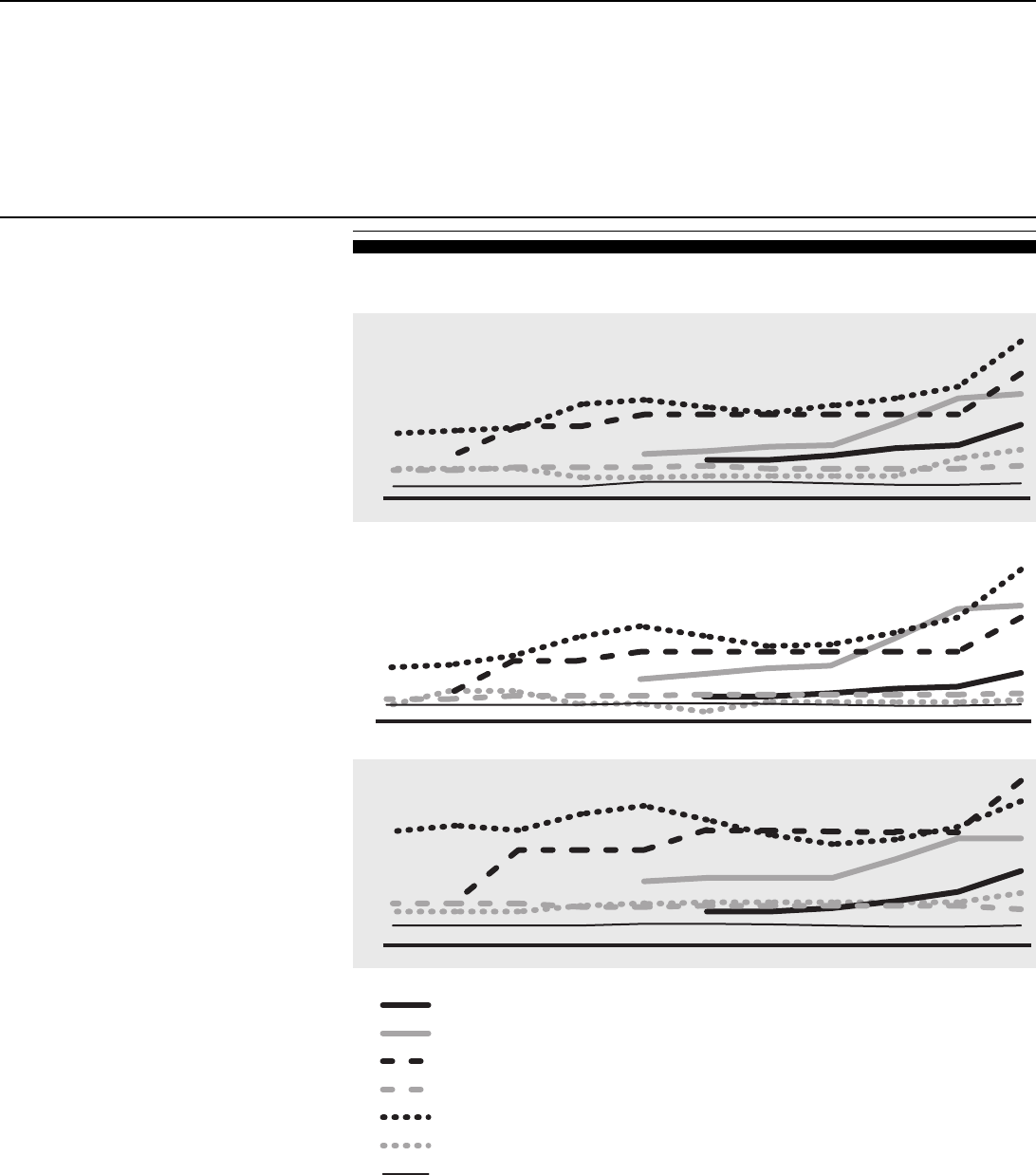
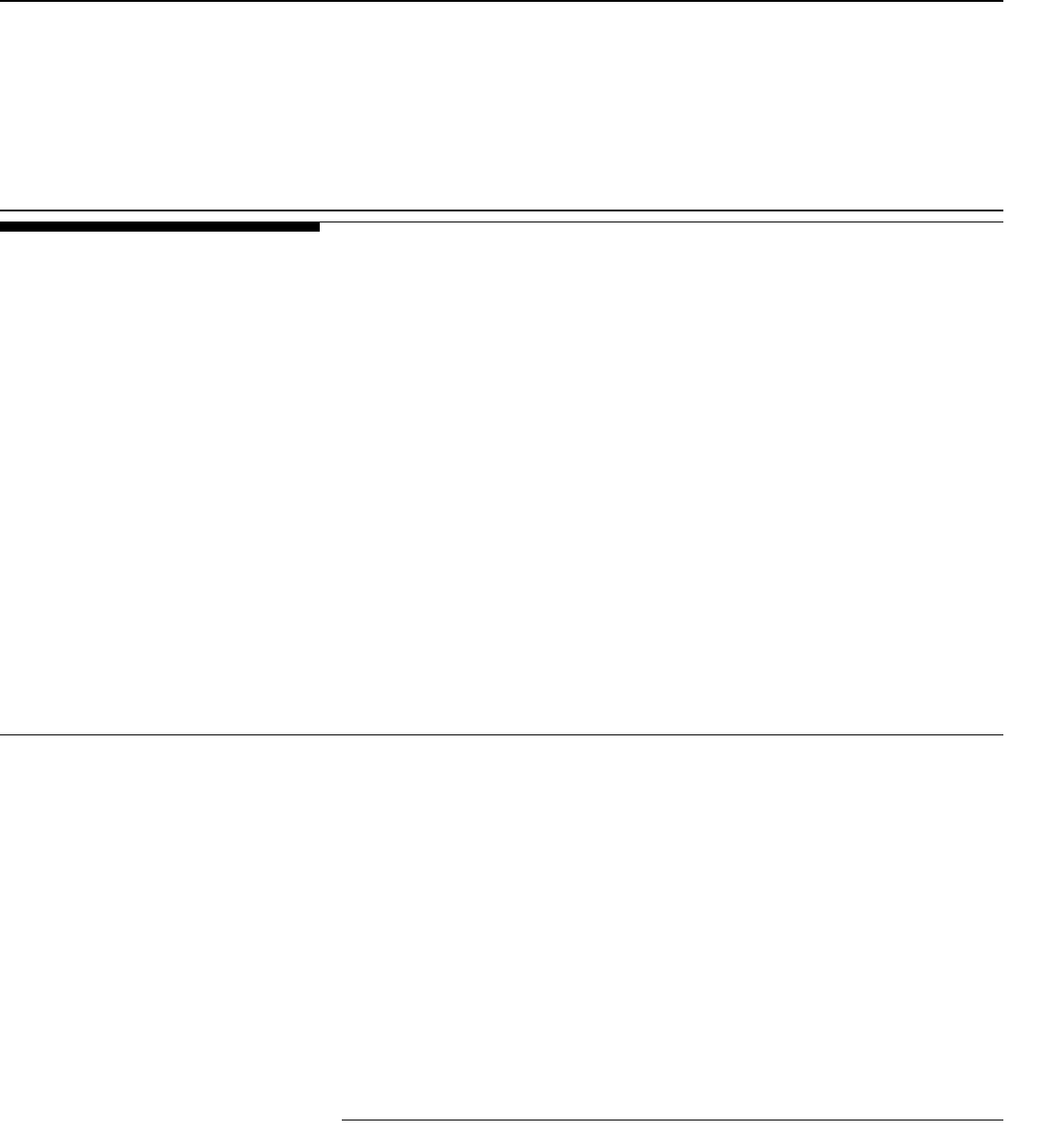
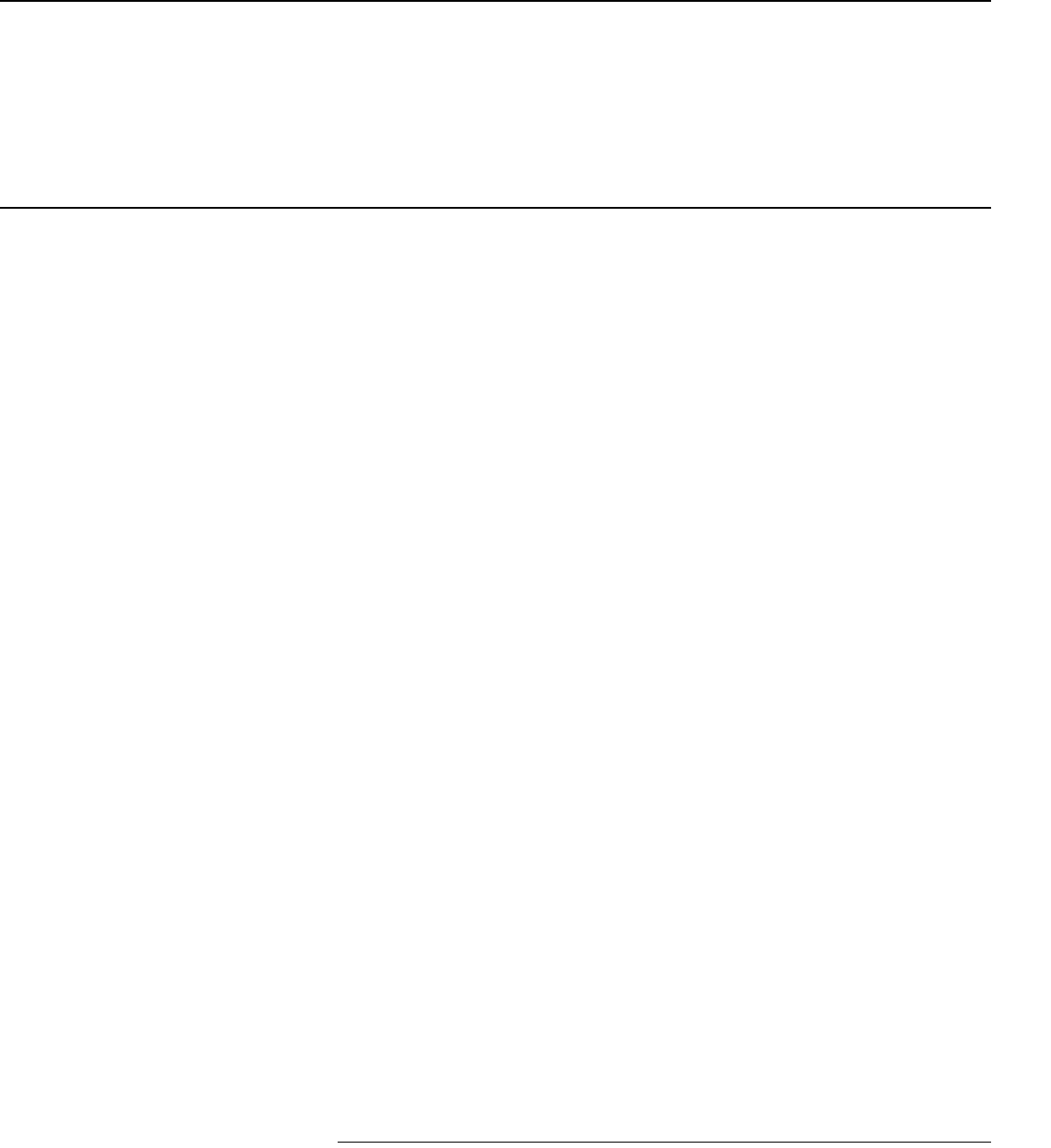
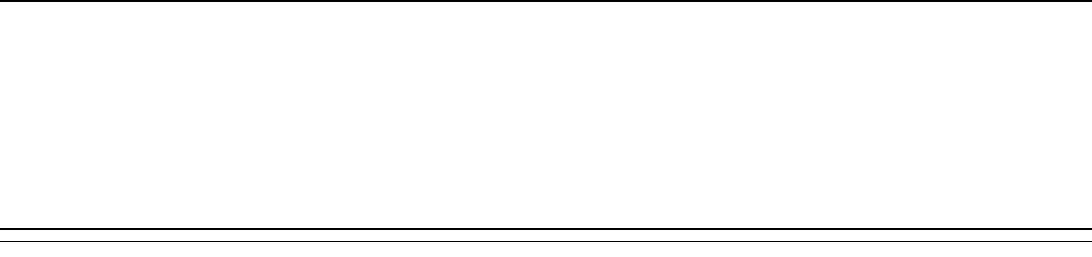
As figure 1 shows, premium base rates varied across our seven sample
states from 1992 to 1998 but for most insurers remained relatively flat.
Beginning in 1999 and 2000, however, most of these insurers began
increasing their rates in larger increments. Many of the increases were
dramatic, ranging as high as 165 percent, although some rates remained
flat. Figure 2 shows the percentage increase in premium rates for the
largest insurers in our seven sample states from 1999 through 2002.
21
In the
Harrisburg area of Pennsylvania, for example, the largest insurer increased
premium base rates dramatically for three specialties: obstetrics/
gynecology (165 percent), general surgery (130 percent), and internal
medicine (130 percent). At the same time, the consumer price index (CPI)
increased by 10 percent. However, in California and Minnesota, premium
base rates for the same specialties rose between 5 and 21 percent and in
some cases fell slightly. The variations in the changes in premium base
rates among our sample states appears to be consistent with the changes in
states outside our sample, with insurers in some states raising premium
rates rapidly after 1999 and insurers in other states raising them very little.
20
In this report, premium rates shown for Pennsylvania include a surcharge for a mandatory
professional liability catastrophe loss fund. Policies purchased from an insurer provide
coverage up to a specific amount, and the loss fund then provides additional coverage. The
amount required to be covered by insurers has been increasing and the amount covered by
the loss fund has been decreasing. In 2002, insurers covered the first $500,000 of any claim,
up to an annual limit of $1.5 million, while the loss fund covered an additional $400,000 per
claim, up to an annual limit of $1.2 million.
21
We determined the largest insurers in each of our seven sample states based on premiums
written in 2001.
Page 11 GAO-03-702 Medical Malpractice Insurance
Figure 1: Premium Base Rates of the Largest Insurers in Seven Selected States for
Three Medical Specialties, 1992–2002
Note: Premium rates shown are annual premium rates for a claims-made policy with a cap of $1 million
per incident and $3 million per year.
Source: GAO analysis of annual surveys by the Medical Liability Monitor.
Pennsylvania Medical Society Liability Insurance
Company in Philadelphia, Pennsylvania (1997-2002)
Texas Medical Liability Trust in El Paso, Texas (1996-2002)
Medical Insurance Exchange of California in Clark County Nevada (1993-2002)
Doctors Company in northern California
First Professionals Insurance Company in Palm Beach County, Florida
Medical Assurance of Mississippi in Mississippi
Midwest Medical Insurance Company in Minnesota
0
20
40
60
80
100
120
20022001200019991998199719961995199419931992
General surgery
Dollars in thousands
0
10
20
30
40
20022001200019991998199719961995199419931992
Internal medicine
Dollars in thousands
0
30
60
90
120
150
20022001200019991998199719961995199419931992
Dollars in thousands
Obstetrics/gynecology
Page 12 GAO-03-702 Medical Malpractice Insurance
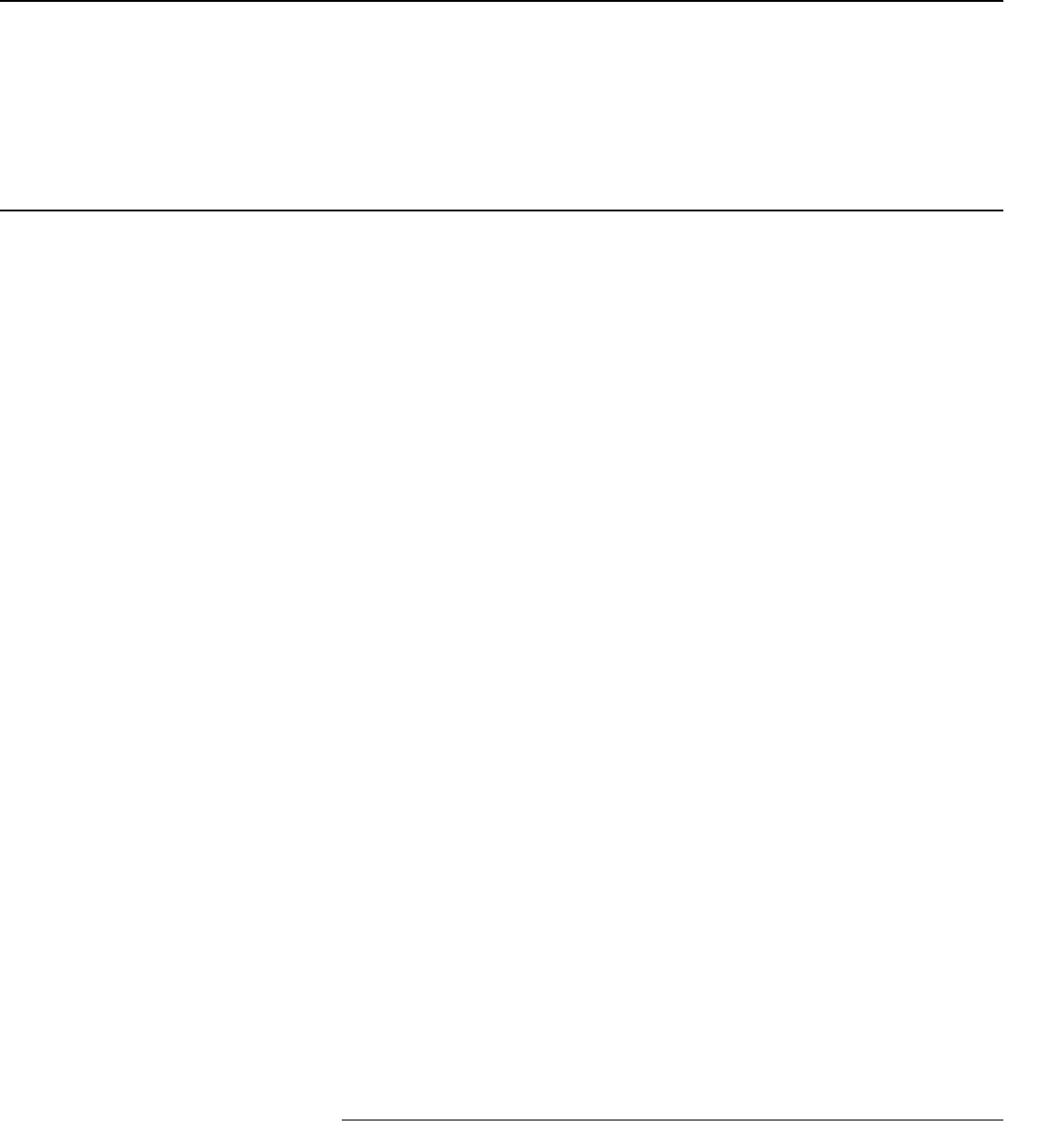
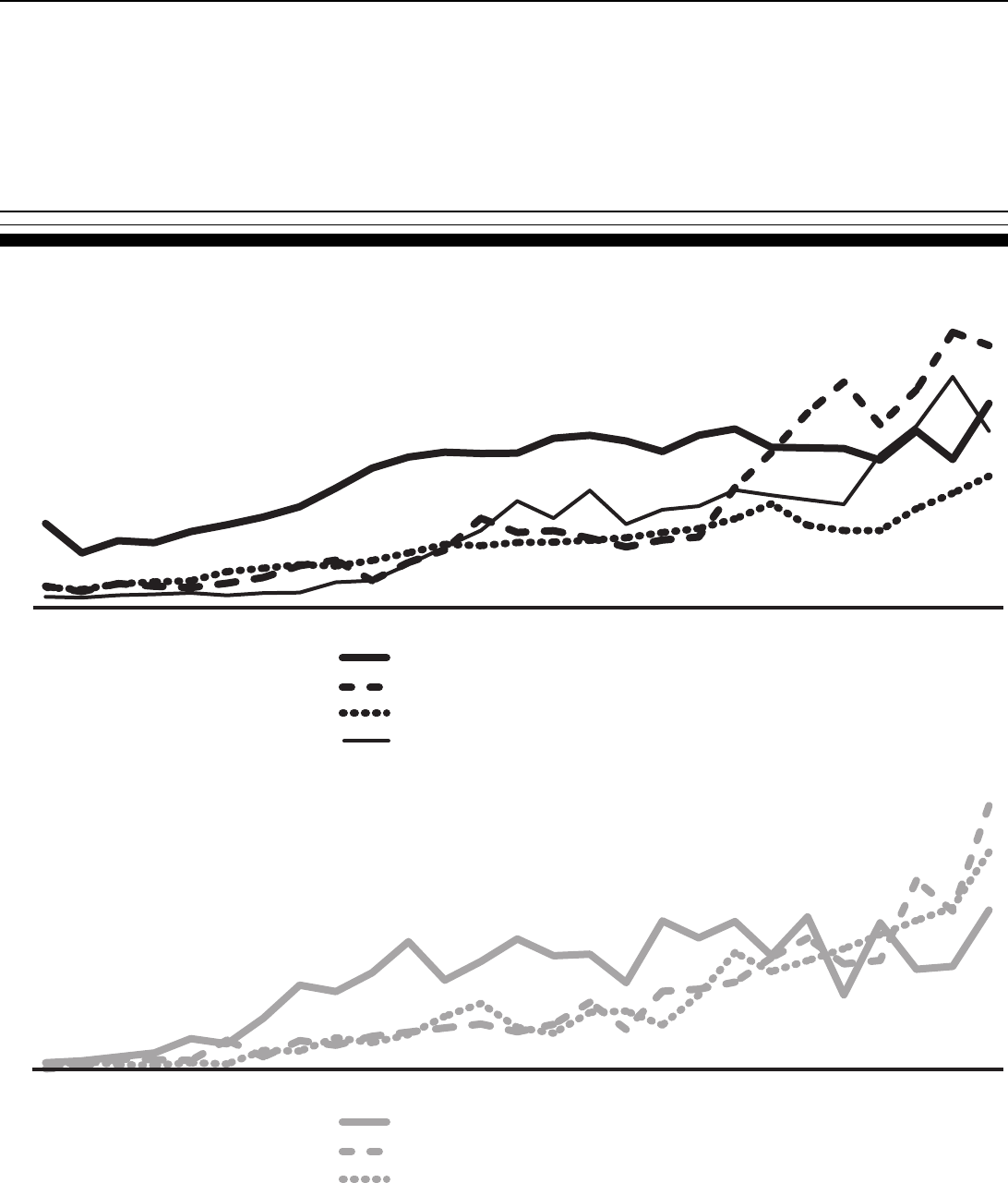
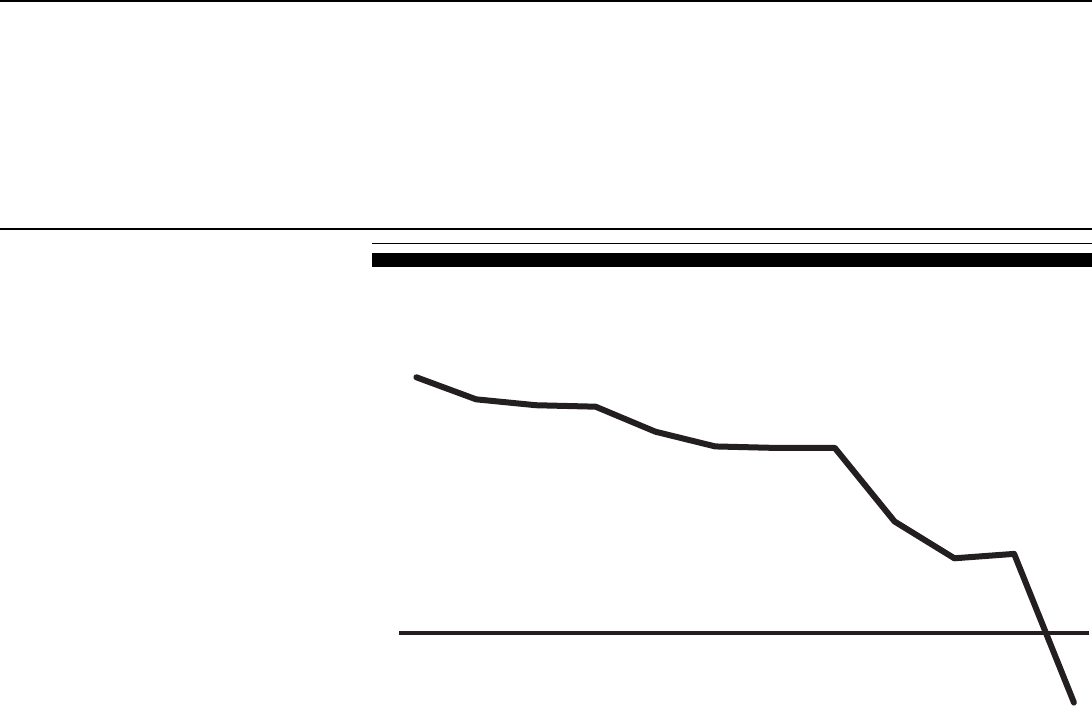
Figure 2: Percentage Changes in Premium Base Rates of the Largest Medical Malpractice Insurers in Seven Selected States for
Three Medical Specialties, 1999–2002
Source: GAO analysis of annual surveys by the Medical Liability Monitor.
Medical Assurance
(Dallas, Texas, area)
Texas Medical Liability
Trust (Amarillo, Texas, area)
Texas Medical Liability
Trust (El Paso, Texas, area)
Pennsylvania Medical Society Liability
Insurance Company (Harrisb
urg area)
Pennsylvania Medical Society Liability
Insurance Company (Pittsburgh area)
Pennsylvania Medical Society Liability
Insurance Company (Philadelphia area)
Medical Insurance Exchange of California
(Nevada, outside of Clark County)
Medical Insurance Exchange
of California
(Clark County, Nevada)
Medical Assurance of
Mississippi (Mississipp
i)
Midwest Medical Insurance
Company (Minnesota)
Medical Assurance (Palm Beach, Florida)
First Professionals Insurance
Company (rest of Florida)
First Professionals Insurance
Company (Dade County, Florida)
Southern California Physician's
Insurance Exchange (Los Angeles Cou
nty)
Southern California Physician's
Insurance Exchange (Sa
n Diego, California)
Medical Insurance Exchange
of California (northern California)
Doctor's Company (northern California)
Cumulative General CPI
Cumulative
Medical Care CPI
General surgery
Internal medicine
Obstetrics/gynecology
-50
0
50
100
150
200
Percentage increase
0
30
60
90
120
150
Percentage increase
0
50
100
150
200
Percentage increase
18
10
14
5
21
15
75 75
51
2
120
50
4
73
82
130
95
104
31
18
10
5
5
21
21
15
15
98 98
52
2
2
10
50
4
73
82
130
108
96
40
18
10
-9
5
43 43
26
21
50
4
99
110
165
60
62
30
Fla. Nev. Tex.Cal. Miss.Minn. Pa.
Fla. Nev. Tex.Cal. Miss.Minn. Pa.
Fla. Nev. Tex.Cal. Miss.Minn. Pa.
Page 13 GAO-03-702 Medical Malpractice Insurance
The Level of Premium Rates
Also Varied across
Specialties and States
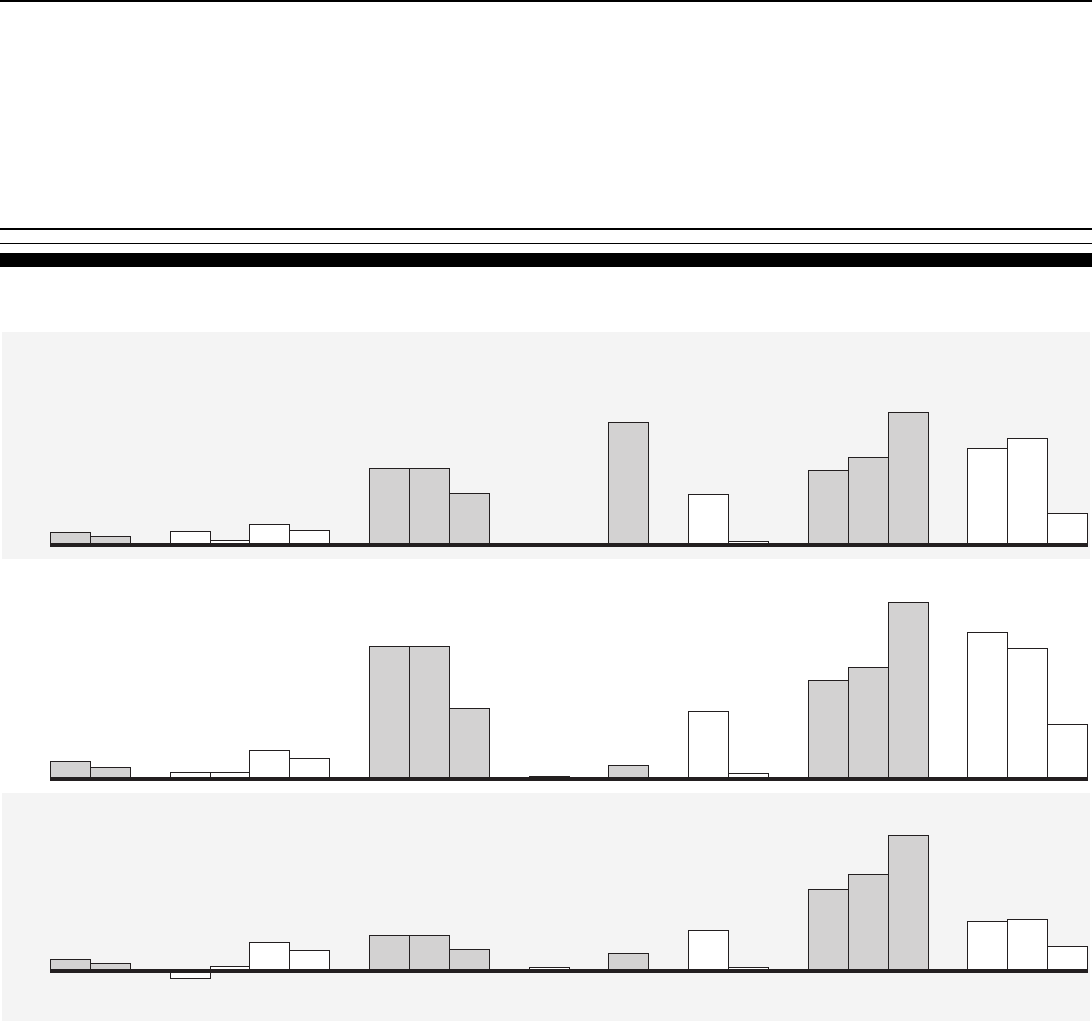
We found that premium rates quoted by insurers in our seven sample states
varied across medical specialties and states. According to some of the
insurers and actuaries we spoke with, the differences in rates reflect the
costs associated with medical malpractice claims against physicians in
particular specialties. Specialties with a high risk of large or frequent losses
on medical malpractice claims will have higher premium rates. For
example, in 2002 the largest medical malpractice insurer in Texas quoted a
base rate for the same level of coverage of $92,000 to obstetricians and
gynecologists, $71,000 to general surgeons, and $26,000 to internists. Figure
3 shows the premium rates quoted by the largest medical malpractice
insurers in our sample states for these three specialties.
22
Premium rates quoted by insurers in our seven sample states for the same
medical specialty also varied across states and geographic areas within
states (see fig. 3). Some of the insurers and actuaries we spoke with told us
that these variations also reflect differences in insurers’ loss experiences in
those venues. As figure 3 shows, the largest insurer in Florida quoted a
premium base rate of $201,000 for obstetricians and gynecologists in Dade
County, while the largest insurer in California quoted a premium based rate
of $36,000 for similar physicians in northern California. Within Florida, the
same large insurer quoted a premium base rate of $103,000 for
obstetricians and gynecologists outside of Dade County—approximately 51
percent of the Dade County rate. Within Pennsylvania, the largest insurer
quoted a premium base rate of $64,000 for doctors in Philadelphia—
approximately 83 percent more than the rate it quoted outside the city.
22
Not all of the insurers included in figs. 3 and 4 are the same, as data that would have
allowed us to complete the same analyses for all of the insurers was not available.
Page 14 GAO-03-702 Medical Malpractice Insurance
Figure 3: 2002 Medical Malpractice Insurance Premium Base Rates of the Largest Insurers in Seven Selected States for Three
Medical Specialties
Note: Premium rates shown are annual premium base rates for coverage under a claims-made policy
with a cap of $1 million per incident and $3 million per year.
Source: GAO analysis of annual surveys by the Medical Liability Monitor.
Texas Medical LiabilityTrust
(Texas's lowest rated territory)
Texas Medical Liability Trust
(Texas's highest rated territory)
First Professionals Insurance
Company (Dade County, Florida)
Southern California Physician's
Insurance Exchange
(southern California)
Norcal
(central California)
Doctor's Company
(northern California)
Pennsylvania Medical Society Liability
Insurance Company (Pittsburgh area)
Pennsylvania Medical Society Liability
Insurance Company (Philadelphia area)
Medical Insurance Exchange of California
(Nevada, outside of Clark County)
Medical Insurance Exchange
of California
(Clark County, Nevada)
Medical Assuran
ce of
Mississippi (Mississippi)
Midwest Medical Insurance
Company (Minnesota)
First Professionals Insurance
Company (rest of Florida)
General surgery
Internal medicine
Obstetrics/gynecology
0
50
100
150
200
250
Dollars in thousands
Dollars in thousands
Dollars in thousands
0
10
20
30
40
50
60
0
50
100
150
200
22
27
34
174
89
10
33
50
28
71
34
85
51
6
12 12
56
29
4
5
11
6
26
13
24
14
31
36
55
201
103
17
45
64
35
92
43
142
85
Fla.
Nev.Tex.Cal. Miss.Minn. Pa.
Nev.Tex.Cal. Miss.Minn. Pa.
Nev.Tex.Cal. Miss.Minn. Pa.
Fla.
Fla.
Page 15 GAO-03-702 Medical Malpractice Insurance
Multiple Factors Have
Contributed to the
Increases in Medical
Malpractice Premium
Rates
Insurers’ losses, declines in investment income, a less competitive climate,
and climbing reinsurance rates have all contributed to rising premium
rates. First, among our seven sample states, insurers’ losses have increased
rapidly in some states, increasing the amount that insurers expect to pay
out on future claims. Second, on the national level insurers’ investment
income has decreased, so that insurance companies must increasingly rely
on premiums to cover costs. Third, some large medical malpractice
insurers have left the market in some states because selling policies was no
longer profitable, reducing the downward competitive pressure on
premium rates that existed through most of the 1990s. Last, reinsurance
rates for some medical malpractice insurers in our seven sample states
have increased substantially, increasing insurers’ overall costs. In
combination, all the factors affecting premium rates and the availability of
medical malpractice insurance contribute to the medical malpractice
insurance cycle of hard and soft markets. While predicting the length, size
and turning points of a cycle may be impossible, it is clear that the
relatively long period of time required to resolve medical malpractice
claims makes the cycles more extreme in this market than in other
insurance markets.
Increased Losses on Claims
Are the Primary Contributor
to Higher Medical
Malpractice Premium Rates
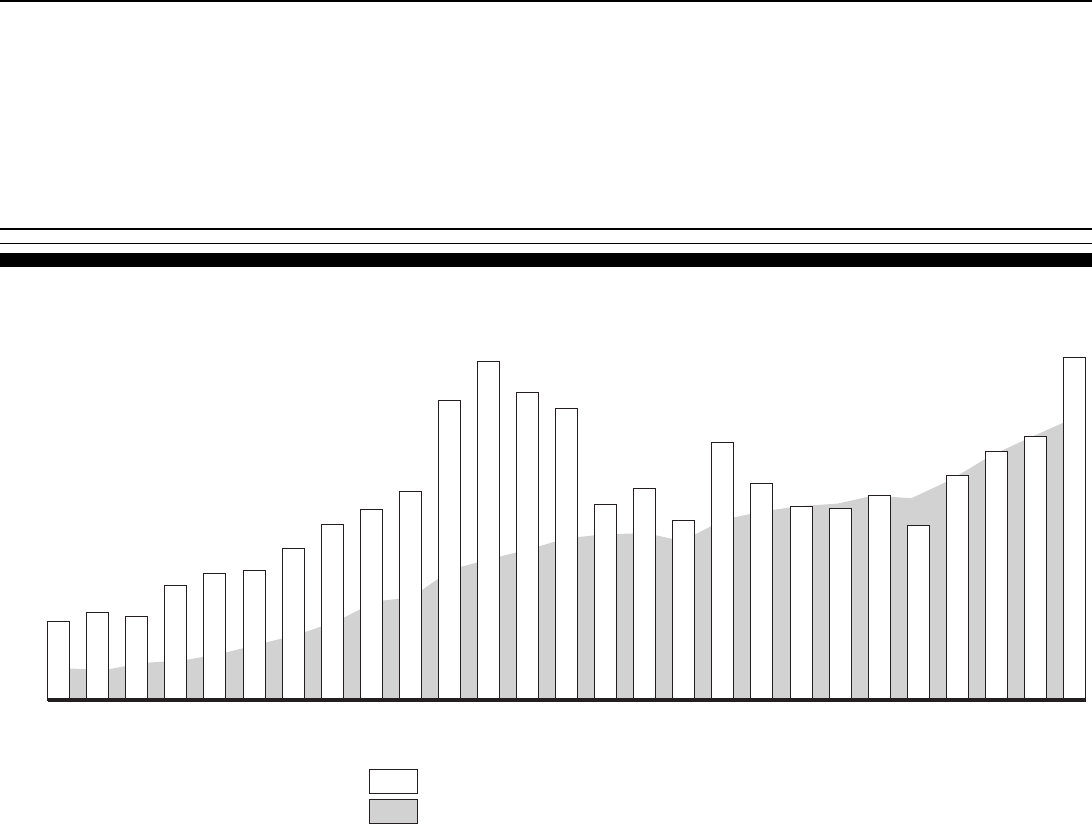
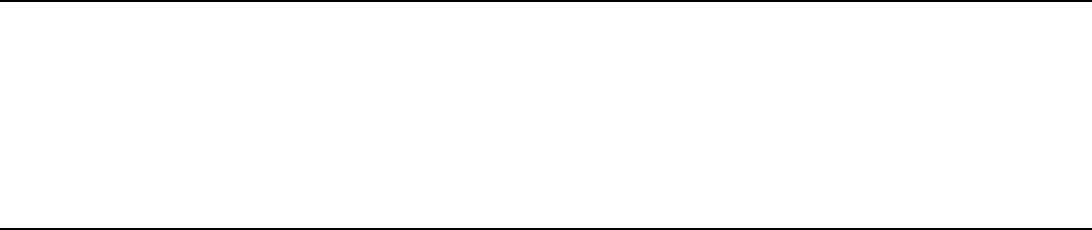
Like premium increases, annual paid losses and incurred losses for the
national medical malpractice insurance market began to rise more rapidly
beginning in 1998.
23
After adjusting for inflation, we found that the average
annual increase in paid losses from 1988 to 1997 was approximately 3.0
percent but that this rate rose to 8.2 percent from 1998 through 2001.
Inflation-adjusted incurred losses decreased by an average annual rate of
3.7 percent from 1988 to 1997 but increased by 18.7 percent from 1998 to
2001. Figure 4 shows paid and incurred losses for the national medical
malpractice market from 1975 to 2001, adjusted for inflation.
23
Over the past several years, some large medical malpractice insurers in some states have
become insolvent. Such insolvencies may have caused aggregate paid losses in those states
to be understated to an unknown extent, because while the insurer may still be paying
medical malpractice claims, they may no longer be reporting those payments to NAIC or
state regulators.
Page 16 GAO-03-702 Medical Malpractice Insurance
Paid and incurred losses give different pictures of an insurer’s loss
experience, and examining both can help provide a better understanding of
an insurer’s losses.
24
Paid losses are the cash payments an insurer makes in
a given year, irrespective of the year in which the claim giving rise to the
payment occurred or was reported. Most payments made in any given year
are for claims that were reported in previous years. In contrast, incurred
losses in any single year reflect an insurer’s expectations of the amounts
that will be paid on claims reported in that year. Incurred losses for a given
year will also reflect any adjustments an insurer makes to the expected
amounts that must be paid out on claims reported during previous years.
That is, as more information becomes available on a particular claim, the
insurer may find that the original estimate was too high or too low and
must make an adjustment. If the original estimate was too high, the
adjustment will decrease incurred losses, but if the original estimate was
too low, the adjustment will increase them.
Incurred losses are the largest component of medical malpractice insurers’
costs. For the 15 largest medical malpractice insurers in 2001—whose
combined market share nationally was approximately 64.3 percent—
incurred losses (including both payments to plaintiffs to resolve claims and
the costs associated with defending claims) comprised, on average, around
78 percent of the insurers’ total expenses. Because insurers base their
premium rates on their expected costs, their anticipated losses will
therefore be the primary determinant of premium rates.
24
According to at least one insurer, the best measure of the results from policies may be the
ultimate paid losses on the claims reported that year, which insurers could compare to the
premiums charged for the policies in question. However, as paid losses are not entirely
known for at least 3 to 5 years after they claims are reported, such information is not
completely available for the years 1998 through 2002.
Page 17 GAO-03-702 Medical Malpractice Insurance
Figure 4: Inflation-Adjusted Paid and Incurred Losses for the National Medical Malpractice Insurance Market, 1975–2001 (Using
the CPI, in 2001 Dollars)
Source: GAO analysis of A.M. Best data.
Dollars in millions
0
1,000
2,000
3,000
4,000
5,000
6,000
7,000
2001
2000
1999
1998
1997
1996
1995
1994
1993
1992
1991
1990
1989
1988
1987
1986
1985
1984
1983
1982
1981
1980
1979
1978
1977
1976
1975
Direct losses incurred in 2001 dollars
Direct losses paid in 2001 dollars
Page 18 GAO-03-702 Medical Malpractice Insurance
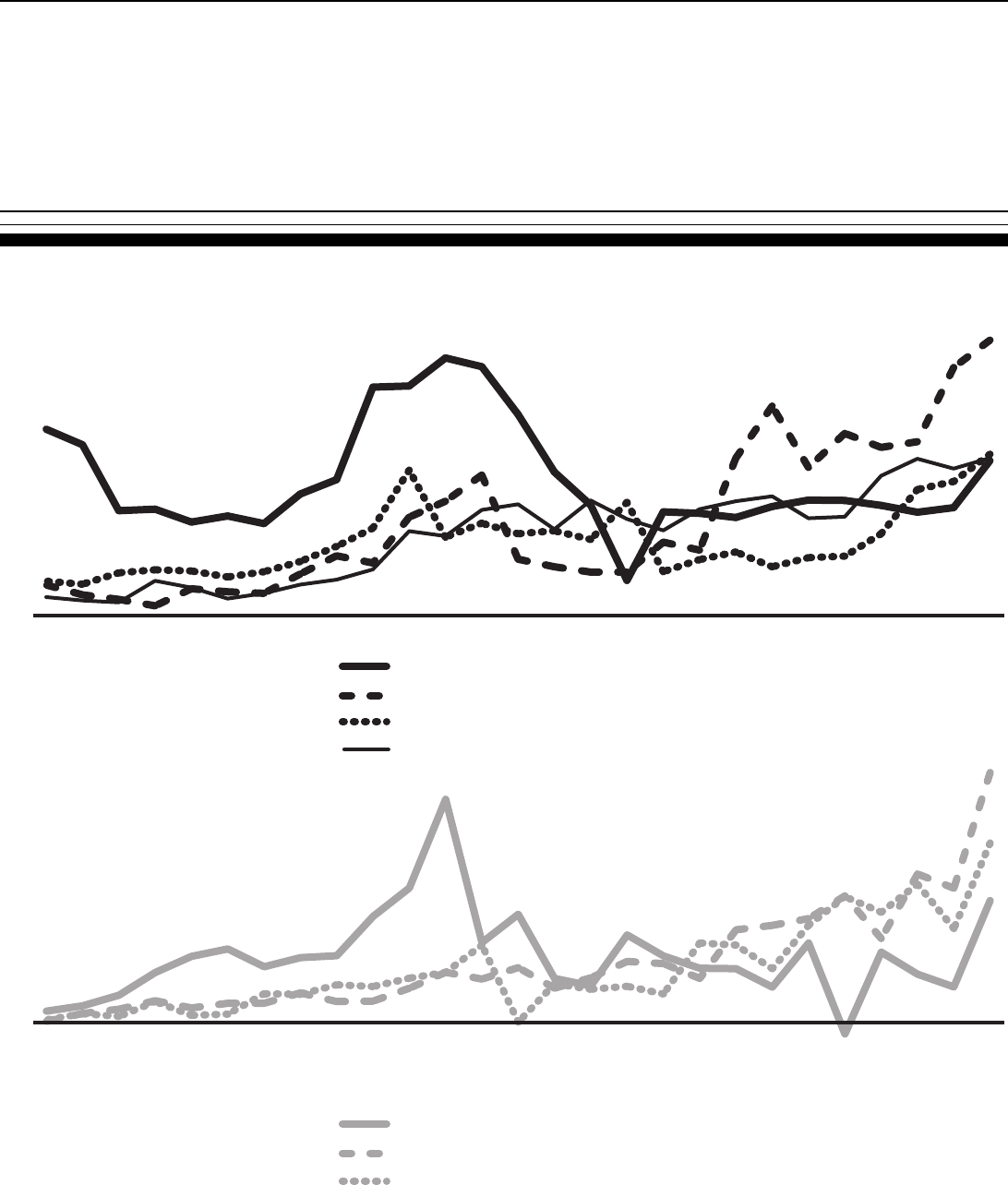
The recent increases in both paid and incurred losses among our seven
sample states varied considerably, with some states experiencing
significantly higher increases than others. From 1998 to 2001, for example,
paid losses in Pennsylvania and Mississippi increased by approximately
70.9 and 142.1 percent, respectively, while paid losses in California and
Minnesota increased by approximately 38.7 and 8.7 percent, respectively
(see fig. 5).
25
Because paid losses in any single year reflect primarily claims
reported during previous years, these losses may not be representative of
claims that were reported during the year the losses were paid.
25
To better show annual changes in the states with smaller total losses, in both figs. 5 and 6
we have separated our seven sample states into two groups, those with smaller total losses
and those with greater total losses.
Page 19 GAO-03-702 Medical Malpractice Insurance
Figure 5: Inflation-Adjusted Aggregate Paid Losses for Medical Malpractice Insurers in Seven Selected States, 1975-2001 (Using
the CPI, in 2001 Dollars)
Source: GAO analysis of A.M. Best data.
Texas
Pennsylvania
Florida
California
Nevada
Mississippi
Minnesota
0
100
200
300
400
500
600
200120001999199819971996199519941993199219911990198919881987198619851984198319821981198019791978197719761975
Dollars in millions
0
10
20
30
40
50
60
70
80
200120001999199819971996199519941993199219911990198919881987198619851984198319821981198019791978197719761975
Dollars in millions
Page 20 GAO-03-702 Medical Malpractice Insurance
From 1998 to 2001, aggregate incurred losses increased by large amounts in
almost all of our seven sample states. As shown in figure 6, the highest
rates of increase in incurred losses over that period were experienced by
insurers in Mississippi (197.5 percent) and Pennsylvania (97.2 percent).
Even in California and Minnesota, states with lower paid losses from 1998
through 2001, insurers experienced increases in incurred losses of
approximately 40.5 and 73.2 percent, respectively, over the same period. As
noted above, incurred losses in any single year reflect insurers’
expectations of future paid losses associated with claims reported in the
current year—that is, claims that will be paid, on average, over the next 3
and one-half years (according to one industry association). And because
insurers’ incurred losses have increased recently, insurers are expecting
their paid losses to increase over the next several years.
Page 21 GAO-03-702 Medical Malpractice Insurance
Figure 6: Inflation-Adjusted Aggregate Incurred Losses for Medical Malpractice Insurers in Seven Selected States, 1975-2001
(Using the CPI, in 2001 Dollars)
Source: GAO analysis of A.M. Best data.
Texas
Pennsylvania
Florida
California
Nevada
Mississippi
Minnesota
Dollars in millions
0
100
200
300
400
500
600
700
800
200120001999199819971996199519941993199219911990198919881987198619851984198319821981198019791978197719761975
Dollars in millions
-20
0
20
40
60
80
100
120
200120001999199819971996199519941993199219911990198919881987198619851984198319821981198019791978197719761975

Page 22 GAO-03-702 Medical Malpractice Insurance
Increased Losses Lead to Higher
Premium Rates
According to actuaries and insurers we spoke with, increased paid losses
raise premium rates in several ways. First, higher paid losses on claims
reported in current or previous years can increase insurers’ estimates of
what they expect to pay out on future claims. Insurers then raise premium
rates to match their expectations. In addition, large losses (particularly
paid losses) on even one or a few individual claims can make it harder for
insurers to predict the amount they might have to pay on future claims.
Some insurers and actuaries we spoke with told us that when losses on
claims are hard to predict, insurers will generally adopt more conservative
expectations regarding losses—that is, they will assume losses will be
toward the higher end of a predicted range of losses. Further, large losses
on individual claims can raise plaintiffs’ expectations for damages on
similar claims, ultimately resulting in higher losses across both claims that
are settled and those that go to trial. As described above, this tendency in
turn can lead to higher expectations of future losses and thus to higher
premium rates. Finally, an increase in the percentage of claims on which
insurers must make payments can increase the amount that insurers expect
to pay on each policy, resulting in higher premium rates. That is, insurers
expecting to pay out money on a high percentage of claims may charge
more for all policies in order to cover the expected increases.
Comprehensive Data on the
Composition and Causes of
Increased Losses Were Lacking
A lack of comprehensive data at the national and state levels on insurers’
medical malpractice claims and the associated losses prevented us from
fully analyzing both the composition and causes of those losses at the
insurer level.
26
For example, comprehensive data that would have allowed
us to fully analyze the severity of medical malpractice claims at the insurer
level on a state-by-state basis did not exist. To begin with, data submitted
by insurers to NAIC on the number of claims reported to insurers are not
broken out by state. Rather, insurers that operate in a number of states
report the number of claims for all their medical malpractice insurance
policies nationwide. Also, while NAIC does collect data that can be used to
measure the severity of claims paid in a single year (number of claims per
state), NAIC began this effort only in 2000. As a result, we could not gather
enough data to examine trends in the severity of paid claims from 1998 to
2002 at the insurer level. Similarly, comprehensive data did not exist that
would have allowed us to analyze claim frequency on a state-by-state basis.
As noted above, data that insurers submit to NAIC on the number of claims
reported were not broken out by state prior to 2000. In addition, insurers do
26
Some additional data on medical malpractice claims, not connected to individual insurers,
were available and were analyzed in a separate report. See GAO-03-836.
Page 23 GAO-03-702 Medical Malpractice Insurance
not submit information on the number of policies in effect or the number of
health care providers insured. Finally, medical associations we spoke with
in our sample states had not compiled accurate data on the number of
physicians practicing within those states. As a result, we could not analyze
changes in the frequency of medical malpractice claims in our sample
states at the insurer level.
Data that would have allowed us to analyze how losses were divided
between settlements and trial verdicts or between economic and
noneconomic damages were also not available. First, insurers do not
submit information to NAIC on the portion of losses paid as part of
settlements and the portion paid as the result of a trial verdict, and no other
comprehensive source of such information exists. However, all eight
insurers and one of the trial lawyers’ associations we spoke with provided
certain estimates about claims. The estimates of three insurers on the
percentage of claims resulting in trial verdicts ranged from 5 to 7 percent.
The estimates of four insurers and 1 state trial lawyers’ association of the
percentage of trial verdicts being decided in favor of the insured defendant
ranged from 70 to 86 percent. The estimates of four insurers and one state
trial lawyers’ association of the portion of claims resulting in payment to
the plaintiff ranged from 14 to 50 percent. Second, no comprehensive
source of information exists on the breakdown of losses between
economic damages, such as medical costs and lost wages, and
noneconomic damages, such as compensation for pain and suffering.
Several of the insurers and trial lawyers’ associations we spoke with noted
that settlement amounts are not formally divided between these two types
of damages and that consistent, comprehensive information on trial
judgments is not collected. Furthermore, while judgment amounts obtained
at trial may be large, several of the insurers we spoke with said that they
most often do not pay amounts beyond a policyholder’s policy limits.
27
Data on the final amounts insurers pay out on individual judgments are not
collected, although they are reported in the aggregate as part of paid losses
in insurers’ financial statements.
27
Some insurers we spoke with told us that they can be liable for amounts beyond a policy’s
limits if the policyholder requests that the insurer settle with the plaintiff for an amount
equal to or less than the policy limit, but the insurer takes the case to trial, loses, and a
judgment is entered in an amount greater than the policy limits. Insurers in California,
Florida, and Texas told us that payments beyond policy limits posed significant issues in
their states.
Page 24 GAO-03-702 Medical Malpractice Insurance
While losses on medical malpractice claims increase as the cost of medical
care and the value of lost wages rise, losses in some states have far
outpaced such inflation. Insurance, legal, and medical industry officials we
spoke with suggested a number of potential causes for such increases.
These potential causes included a greater societal propensity to sue; a
“lottery mentality,” where a lawsuit is seen as an easy way to get a large
sum of money; a sicker, older population; greater expectations for medical
care because of improved technology; and a reduced quality of care and the
breakdown of the doctor-patient relationship owing, for example, to factors
such as the increasing prevalence of managed care organizations. While we
could not analyze such potential causes for increased losses,
understanding them would be useful in developing strategies to address
increasing medical malpractice premium rates. That is, because losses on
claims have such a profound effect on premium rates, understanding the
reasons those losses have increased could make it easier to devise actions
to control the rise in premium rates.
28
Medical Malpractice
Insurers’ Investment
Income Has Decreased
State laws restrict medical malpractice insurers to conservative
investments, primarily bonds. In 2001, the 15 largest writers of medical
malpractice insurance in the United States
29
invested, on average, around
79 percent of their investment assets in bonds, usually some combination
of U.S. Treasury, municipal, and corporate bonds. While the performance of
some bonds has surpassed that of the stock market as a whole since 2000,
annual yields on selected bonds since 2000 have decreased steadily since
then (table 1).
28
State laws for resolving medical malpractice claims may also affect the extent to which
losses increase in a particular state. The effect of state laws on losses and premium rates is
discussed in greater detail in GAO-03-836.
29
As reported by A.M. Best. These insurers included a combination of commercial
companies and physician-owned nonprofit insurers. Some of these insurers sold more than
one line of insurance, and changes in returns on investments might not be reflected equally
in the premium rates in each of those lines.
Page 25 GAO-03-702 Medical Malpractice Insurance
Table 1: Annual Yields for Selected Bonds, 1995–2002, and Average Return on Investment Assets, 1997–2002, for the 15 Largest
Writers of Medical Malpractice Insurance in 2001
Source: GAO analysis of data from A.M. Best, the Federal Reserve, and the Bond Market Association.
a
Data for 1995 and 1996 were not readily available.
b
Complete information was not available for the same companies in 2002. The 2002 average return on
investment was estimated based on the average bond yield and the average ratio of the bond yield to
the insurer’s return on investment.
We analyzed the average investment returns of the 15 largest medical
malpractice insurers of 2001 and found that the average return fell from
about 5.6 percent in 2000 to an estimated 4.0 percent in 2002. However,
none of the companies experienced a net loss on investments at least
through 2001, the most recent year for which such data were available.
Additionally, almost no medical malpractice insurers overall experienced
net investment losses from 1997 to 2001.
Medical malpractice insurers are required by state insurance regulations to
reflect expected investment income in their premium rates. That is,
insurers are required to reduce their premium rates to consider the income
they expect to earn on their investments. As a result, when insurers expect
their returns on investments will be high, as returns were during most of
the 1990s, premium rates can remain relatively low because investment
income covers a larger share of losses on claims. Conversely, when
insurers expect their returns on investments will be lower—as returns have
been since around 2000—premium rates rise in order to cover a larger
share of losses. During periods of relatively high investment income,
insurers can lose money on the underwriting portion of their business yet
1995 1996 1997 1998 1999 2000 2001 2002
5-Year U.S. Treasury
securities 6.38 6.18 6.22 5.15 5.55 6.16 4.56 3.82
10-Year U.S. Treasury
securities 6.57 6.44 6.35 5.26 5.65 6.03 5.02 4.61
5-Year AAA-rated municipal
bonds 4.57 4.41 4.34 3.97 4.18 4.72 3.63 3.16
10-Year AAA-rated municipal
bonds 5.04 4.91 4.75 4.31 4.62 4.97 4.28 4.05
5-Year AAA-rated corporate
bonds 6.71 6.49 6.52 5.61 6.17 6.96 5.24 4.45
10-Year AAA-rated corporate
bonds 6.93 6.77 6.66 5.74 6.38 7.09 5.92 5.42
Average return on investment
assets for 15 largest insurers
aa
5.6 5.5 5.2 5.6 5.0 4.0
b
Page 26 GAO-03-702 Medical Malpractice Insurance
still make a profit. That is, losses from medical malpractice claims and the
associated expenses may exceed premium income, but income from
investments can still allow the insurer to operate profitably. Insurers are
not allowed to increase premium rates to compensate for lower-than-
expected returns on past investments but must consider only prospective
income from investments.
None of the insurers that we consulted regarding this issue told us
definitively how much the decreases in investment income had increased
premium rates. But we can make a rough estimate of the relationship
between return on investment and premium rates. When investment
income decreases, holding all else constant, income from premium rates
must increase by an equal amount in order for the insurer to maintain the
same overall level of income. Thus the total amount of investment assets
relative to premium income determines how much rates need to rise to
compensate for lost investment income. Table 2 presents a hypothetical
example. An insurer has $100,000 in investment assets and in the previous
year received $25,000 in premium income, for a ratio of investment assets
to premium income of 4 to 1. If the return on investments drops 1
percentage point and all else remains constant, the insurer must raise
premium rates by 4 percent in order to compensate for the reduced
investment income. If the return on investments drops by 2 percentage
points, premium rates must rise by 8 percent to compensate.
Page 27 GAO-03-702 Medical Malpractice Insurance
Table 2: Hypothetical Example of How Premium Rates Change When the Return on
Investments Falls
Source: GAO analysis.
Note: The examples given assume that all else holds constant and that the insurer must obtain the full
amount of additional funds required in the following year, even though the insurer would earn interest
on those funds and thus would not need to increase premium rates by the full amount. Such an
assumption may overstate the extent to which premium rates must be increased. The examples also
do not take into account the fact that insurers look prospectively at trends in interest rates when
estimating their anticipated investment income. By not taking into account a downward trend in interest
rates, such as the one that has existed since 2000, our examples may understate the needed increase.
This relationship can be applied to the 15 largest medical malpractice
insurers—countrywide—from 2001. Data show that in 2001 the insurers’
total investment assets were, on average, around 4.5 times as large as the
amount of premium income they earned for that year. Applying the
relationship established above and holding other factors constant, a drop
of 1 percentage point in return on investments would translate into roughly
a 4.5 percent increase in premium rates.
30
As a result, if nothing else
changed, the approximately 1.6 percentage point drop in the return on
investments these insurers experienced from 2000 through 2002 would
have resulted in an increase in premium rates of around 7.2 percent over
the same 2-year period.
Example 1 Example 2 Example 3
(a) Total investment assets $100,000 $100,000 $100,000
(b) Original total premium
income $25,000 $25,000 $25,000
(c) Percentage point drop
in return on investments 1% 2% 3%
(d) Drop in investment
income [(a) x (c)] $1,000 $2,000 $3,000
Total premium income
required to make up for
drop in investment income
[(b) + (d)] $26,000 $27,000 $28,000
Percentage increase in
premium income required
[(d) / (b) x 100] 4% 8% 12%
30
Insurers in states where it takes more time to resolve medical malpractice claims would be
more affected by changes in interest rates than insurers in states where it takes less time to
resolve claims.
Page 28 GAO-03-702 Medical Malpractice Insurance
Downward Pressure on
Premium Rates Has
Decreased as Profitability
Has Declined
Since 1999, the profitability of the medical malpractice insurance market as
a whole has declined—even with increasing premium rates—causing some
large insurers to pull out of this market, either in certain states or
nationwide. Because fewer insurers are offering this insurance, there is less
price competition and thus less downward pressure on premium rates.
According to some industry and regulatory officials in our seven sample
states, price competition during most of the 1990s kept premium rates from
rising between 1992 and 1998, even though losses generally did rise. In
some cases, rates actually fell. For example, during this period premium
rates for obstetricians and gynecologists covered by the largest insurer in
Florida—a state where these physicians are currently seeing rapid
premium rate increases—actually decreased by approximately 3.1 percent.
Some industry participants we spoke with told us that, in hindsight,
premium rates charged by some insurers during this period may have been
lower than they should have been and, after 1998, began rising to a level
more in line with insurers’ losses on claims. Some industry participants
also pointed out that this pricing inadequacy was masked to some extent by
insurers’ adjustments to expected losses on claims reported during the late
1980s as well as their high investment income. For many insurers the
incurred losses associated with the policies sold during the late 1980s
turned out to be higher than the actual losses for the same policies,
resulting in high levels of reserves. During the 1990s, as insurers eliminated
these redundant reserves by adjusting their current loss reserves for these
previous overestimates, current calendar year incurred losses fell and
reported income increased. These adjustments, together with relatively
high levels of investment income, allowed insurers to keep premium rates
flat and still remain profitable.
Selling Medical Malpractice
Insurance Has Become Less
Profitable
Beginning in the late 1990s, medical malpractice insurers as a whole began
to see their profits fall. Figure 7 shows the return on surplus—also called
return on equity—for the medical malpractice insurance industry as a
whole. Profitability began declining faster in 1998 and in 2001 dropped
considerably even as premium rates were increasing in many states,
resulting in a negative rate of return, or loss. Some of the factors pushing
premium rates upward were also factors in insurers’ declining profitability:
higher losses on medical malpractice claims, higher reinsurance costs, and
falling investment income.
Page 29 GAO-03-702 Medical Malpractice Insurance
Figure 7: Net Profit or Loss as a Percentage of Net Worth for Medical Malpractice
Insurance Companies Nationwide, 1990–2001
Medical malpractice insurers in some of our sample states have
experienced particularly low levels of profitability since around 1998 (see
fig. 8). The loss ratio reported here is the ratio of incurred losses, not
including other expenses (often referred to as loss adjustment expenses)
related to resolving those claims, to the amount of premiums earned in a
given year. Loss ratios above 100 percent indicate that an insurer has
incurred more losses than premium payments, a sign of declining
profitability. Loss ratios in all seven sample states have increased since
1998, and except for California, all had loss ratios of more than 100 percent
for 2001.
Source: GAO analysis of NAIC data.
-5
0
5
10
15
20
200120001999199819971996199519941993199219911990
Percentage of net worth
17.4
15.9
15.5
15.4
13.7
12.7
12.6 12.6
7.6
5.1
5.4
-4.7
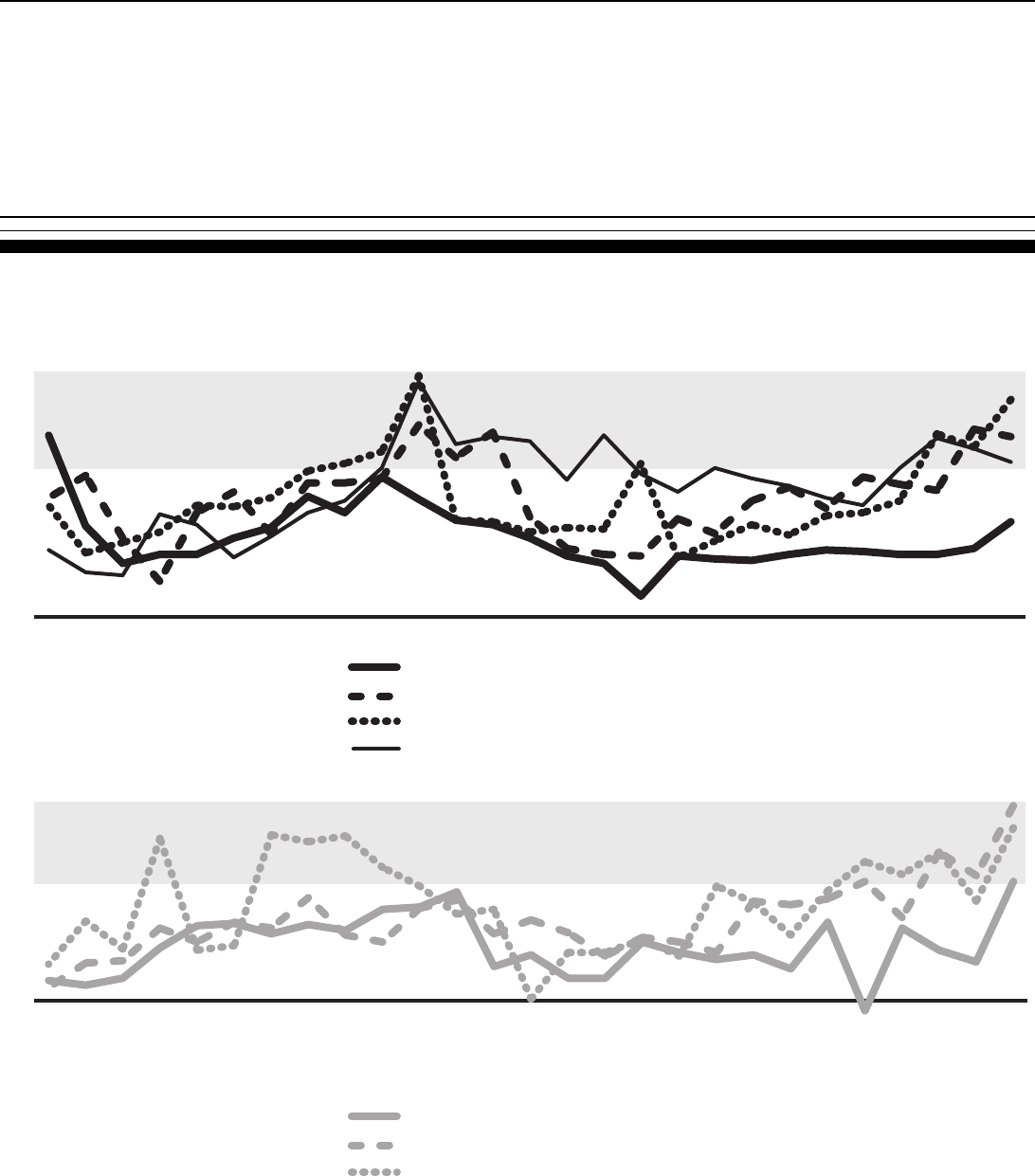
Page 30 GAO-03-702 Medical Malpractice Insurance
Figure 8: Aggregate Incurred Losses as a Percentage of Premiums Earned for Medical Malpractice Insurers in Seven Selected
States, 1975–2001
Note: Incurred losses used in this figure do not include other expenses related to resolving claims or
loss adjustment expenses.
Source: GAO analysis of A.M. Best data.
Texas
Pennsylvania
Florida
California
Nevada
Mississippi
Minnesota
Percentage
0
50
100
150
200
200120001999199819971996199519941993199219911990198919881987198619851984198319821981198019791978197719761975
Percentage
-50
0
50
100
150
200
200120001999199819971996199519941993199219911990198919881987198619851984198319821981198019791978197719761975
Percentages above 100 indicate that
losses from medical malpractice claims
exceeded premiums for the year.
Percentages above 100 indicate that
losses from medical malpractice claims
exceeded premiums for the year.
Page 31 GAO-03-702 Medical Malpractice Insurance
As Profits Have Fallen, Insurers
Have Left the Medical
Malpractice Market
This declining profitability has caused some large insurers either to stop
selling medical malpractice policies altogether or to reduce the number
they sell. For example, beginning in 2002 the St. Paul Companies—
previously the second-largest medical malpractice insurer in the United
States—stopped writing all medical malpractice insurance because of
declining profitability. In 2001, St. Paul had sold medical malpractice
insurance in every state and was the largest or second-largest seller in 24
states. St. Paul was not alone. Other large insurers have also stopped
selling medical malpractice insurance in since 1999: PHICO Insurance
Company, which sold insurance primarily in six states, including Florida,
Pennsylvania, and Texas; MIIX Insurance Company, which sold insurance
primarily in five states, including New Jersey and Pennsylvania; and
Reciprocal of America, which sold insurance primarily in six states,
including Alabama, Mississippi, and Virginia. Other insurers reduced the
number of states in which they sold medical malpractice insurance: SCPIE
Indemnity Company, which in March 2003 essentially stopped selling
insurance outside of California, and First Professionals Insurance
Company, which has said that beginning in 2003 it will essentially stop
selling insurance outside of Florida.
When a large insurer leaves a state insurance market, the supply of medical
malpractice insurance decreases, and the remaining insurers may not need
to compete as much on the basis of price. In addition, the remaining
insurers are limited in the amount of insurance they can supply to fill the
gap, because state insurance regulations limit the amount of insurance they
can write relative to their surplus (the amount by which insurers’ assets
exceed their liabilities). For mutual, nonprofit insurers, increasing the
surplus can be a slow process, because surplus must generally be built
through profits or by obtaining additional funds from policyholders.
Commercial insurers can obtain funds through capital markets, but even
then, convincing investors to invest funds in medical malpractice insurance
when profits are falling can be difficult.
Remaining Insurers Have
Increased Prices to Reflect
Expected Losses
According to industry participants and observers, as the competitive
pressures on premium rates decreased, it appears that insurers were able
to more easily and more quickly raise premium rates to a level more in line
with their expected losses. That is, absent competitive pressure that may
have caused insurers to keep premium rates at lower levels, which in
hindsight were perhaps too low for the ultimate losses the insurers would
have to pay, it appears that insurers were able to raise premium rates to
match their loss expectations. As noted earlier, losses increased to a great
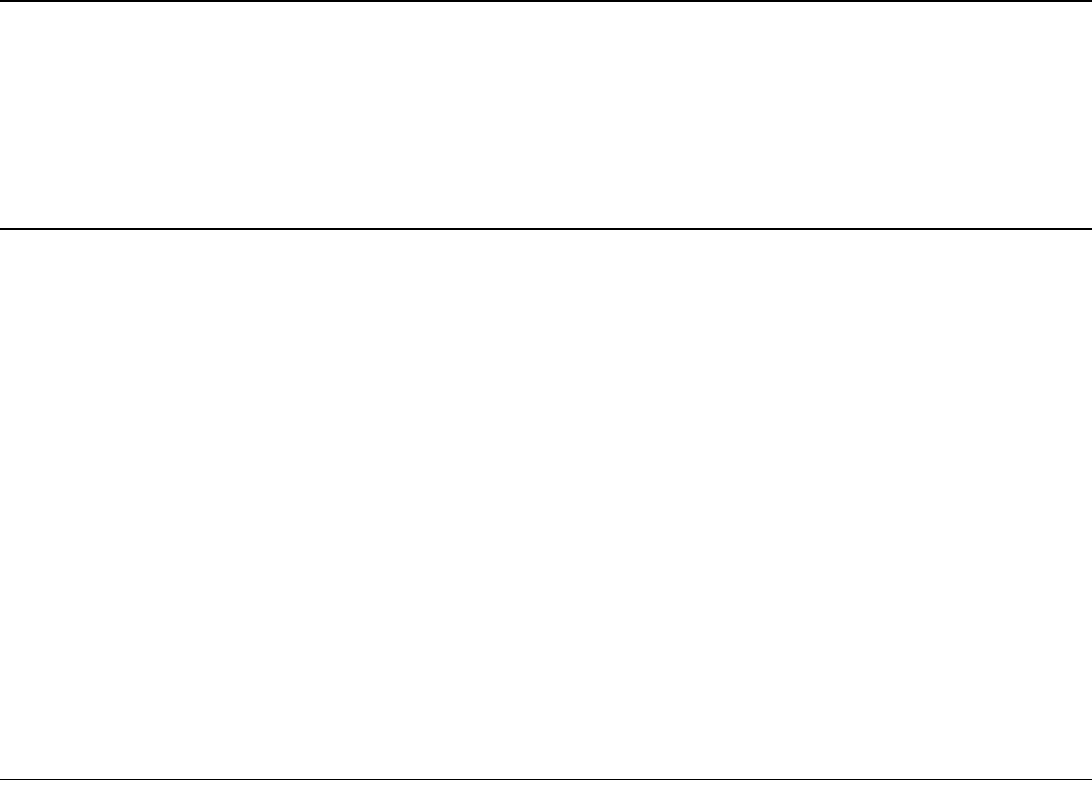
Page 32 GAO-03-702 Medical Malpractice Insurance
extent in some states, and thus some insurers may have increased premium
rates dramatically.
While it appears clear that a reduction in price competition has allowed
insurers to more easily and more quickly increase premium rates to a level
more in line with insurers’ expected losses, we identified at least three
factors that seem to suggest that these premium rates are not inconsistent
with expected losses. First, if the higher premium rates were above what
was justified by insurers’ expected losses, profitability would be increasing.
But profits are not increasing, indicating that insurers are not charging and
profiting from excessively high premium rates. Second, according to some
industry participants we spoke with, physician-owned insurers have little
incentive to overcharge their policyholders because those insurers
generally return excess earnings to their policyholders in the form of
dividends. Third, in most states the insurance regulators have the authority
to deny premium rate increases they deem excessive. While the
information that state regulators require insurers to submit as justification
for premium rate increases varies across states, in general it includes data
on expected losses.
Reinsurance Premium Rates
Have Increased
A further reason for recent increases in medical malpractice premium rates
in our seven sample states was that the cost of reinsurance for these
insurers has also increased, increasing the total expenses that premium
and other income must cover. Insurers in general purchase reinsurance, or
excess loss coverage, to protect themselves against large unpredictable
losses. Medical malpractice insurers, particularly smaller insurers, depend
heavily on reinsurance because of the potential high payouts on medical
malpractice claims.
Reinsurance industry officials and medical malpractice insurers we spoke
with told us that reinsurance premium rates have increased for two
reasons. First, reinsurance rates overall have increased as a result of
reinsurers’ losses related to the terrorist attacks of September 11, 2001.
Second, reinsurers have seen higher losses from medical malpractice
insurers and have raised rates to compensate for the increased risk
associated with providing reinsurance to the medical malpractice market.
Some insurers and industry participants told us that reinsurance premium
rates had risen substantially since 1998, with the increases ranging from 50
to 100 percent. Other insurers told us that in order to keep their
reinsurance premium rates down, they increased the dollar amount on any
loss at which reinsurance would begin, essentially increasing the
Page 33 GAO-03-702 Medical Malpractice Insurance
deductible. Thus, while reinsurance rates may not have increased, the
amount of risk the medical malpractice insurers carry did. One insurer
estimated that while its reinsurance rates had increased approximately 50
percent from 2000 to 2002, this increase had resulted in only a 2 to 3
percent increase in medical malpractice premium rates.
The Medical Malpractice
Insurance Market Moves
through Hard and Soft
Insurance Markets
All of the factors affecting premium rates and availability contribute to the
length and amplitude of the medical malpractice insurance cycle. Like
other property-casualty insurance markets, the medical malpractice
market moves through cycles of “hard” and “soft” markets. Hard markets
are generally characterized by rapidly rising premium rates, tightened
underwriting standards, narrowed coverage, and often by the departure of
some insurers from the market. In the medical malpractice market, some
market observers have characterized the period from approximately 1998
to the present as a hard market. (Previous hard markets occurred during
the mid-1970s and mid-1980s.) Soft markets are characterized by slowly
rising premium rates, less stringent underwriting standards, expanded
coverage, and strong competition among insurers. The medical malpractice
market from 1990 to 1998 has been characterized as a soft market.
According to a series of studies sponsored and published by NAIC in 1991,
such cycles have been present in the property-casualty insurance market
since at least 1926, and until the mid-1970s lasted for an average of
approximately 6 years from the peak of one hard market to the next.
31
However, the cycle that began at the peak of the hard market in 1975 lasted
for around 10 years. The current cycle has lasted for around 17 years—
since 1985—and it is not yet clear that the current hard market has peaked.
Cycles in the Medical
Malpractice Market Tend to Be
Volatile
The medical malpractice insurance market appears to roughly follow the
same cycles as the overall property-casualty insurance market, but the
cycles tend to be more volatile—that is, the swings are more extreme. We
analyzed the swings in insurance cycles for the medical malpractice market
and for the entire property-casualty insurance markets using annual loss
ratios based on incurred losses (see fig. 9). Our analysis showed that
annual loss ratios for medical malpractice insurers tended to swing higher
or lower than those for property-casualty insurers as a whole, reflecting
more extreme changes in insurers’ expectations. Because premium rates
31
National Association of Insurance Commissioners, Cycles and Crises in
Property/Casualty Insurance: Causes and Implications for Public Policy (Kansas City,
Mo.: 1991).

Page 34 GAO-03-702 Medical Malpractice Insurance
are based largely on insurers’ expectations of losses, premium rates will
fluctuate as well.
Figure 9: Incurred Losses as a Percentage of Premium Income for Medical Malpractice Insurers and Property-Casualty Insurers
Nationwide, 1976–2001
The medical malpractice insurance market is more volatile than the
property-casualty insurance market as a whole because of the length of
time involved in resolving medical malpractice claims and the volatility of
the claims themselves. Several years may pass before insurers know and
understand the profits and losses associated with policies sold in a single
year. As a result, insurers may not know the full effects of a change in an
underlying factor, such as losses or return on investments, for several
years. So while insurers in other markets that do not have protracted
claims resolutions can adjust loss estimates and premium rates more
quickly to account for a change in an underlying factor, medical
malpractice insurers may not be able to make adjustments for several
years. In the interim, medical malpractice insurers may unknowingly be
under- or over-pricing their policies.
Percentages above 100 indicate that
losses from medical malpractice claims
exceeded premiums for the year.
All property casualty insurers
Medical malpractice insurers
Percentage of premiums
Source: GAO analysis of A.M. Best and National Association of Insurance Commissioners data.
40
60
80
100
120
20012000199919981997199619951994199319921991199019891988198719861985198419831982198119801979197819771976
Page 35 GAO-03-702 Medical Malpractice Insurance
When insurers do fully understand the effects of a change in an underlying
factor, they may need to make large adjustments in loss estimates and
premium rates. As a result, premium rates in the medical malpractice
insurance market may move more sharply than premium rates in other
lines of property-casualty insurance. For example, if insurers have been
unknowingly overestimating their losses and overpricing their policies, as
some insurers told us happened during the late 1980s, large liabilities build
up to cover the losses. When the insurers realize their estimates have been
too high, they must reduce those liabilities to reflect their losses accurately.
Reducing liabilities also reduces incurred losses and therefore increases
insurers’ income, allowing insurers to charge lower premium rates even in
the face of increased losses and still maintain profitable operations—a
point some insurers made about the 1990s. But when the liability account
has been reduced sufficiently and income is no longer increasing as a result
of this adjustment, insurers may need to raise premium rates to stay
profitable.
The competition that can exist during soft markets and periods of high
investment income can further exacerbate swings in premium rates. As
noted earlier, competition among insurers can put downward pressure on
premium rates, even to the point at which the rates may, in hindsight,
become inadequate to keep an insurer solvent. When the insurance market
hardens, some insurers may leave the market, removing the downward
pressure on premium rates and allowing insurers to raise premium rates to
the level that would have existed without such competition. Because
competition may have kept rates low, the resulting increase in premium
rates that accompanies a transition to a hard market may be greater than it
would have been otherwise.
According to some industry experts, periods of high investment income
can bolster the downward pressure that exists during soft markets. That is,
high investment income can contribute to the increased profitability of an
insurance market. This profitability can, in turn, cause insurers to compete
for market share in order to take advantage of that profitability, thereby
forcing premium rates even lower. In addition, according to these industry
experts, high investment income allows insurers to keep premium rates
low for long periods of time, even in the face of increasing losses, because
investment income can be used to replace premium income, allowing
insurers to meet expenses. But if interest rates drop at the same time the
market hardens (and reduced interest rates can be a contributor to the
movement to hard market), insurers may have to increase premium rates
Page 36 GAO-03-702 Medical Malpractice Insurance
much more in a shorter period of time than they would have if investment
income had not allowed premium rates to remain lower to begin with.
Predicting and Moderating the
Cycle is Difficult
While the medical malpractice insurance market will likely move through
more soft and hard markets in the future, predicting when such moves
might occur or the extent of premium rate changes is virtually impossible.
For example, the timing and extent of the unexpected changes in the losses
that some researchers believe are responsible for hard markets are
virtually impossible to predict. In addition, as we have seen, many factors
affect premium rates, and it is just as difficult to predict the extent of any
future changes these factors might undergo. While interest rates may be
high during soft markets, it is not possible to predict how much higher they
might be in the future and thus what effect they might have on premium
rates. Predicting changes in losses on medical malpractice claims would be
even harder, given the volatility of such losses. Further, some of the factors
affecting premium rates, such as losses and competition, vary across
states, and the effect of soft or hard markets on premium rates in one state
could not be generalized to others. Finally, other conditions affecting
premium rates have changed since earlier hard and soft markets, limiting
our ability to make accurate comparisons between past and future market
cycles.
Similarly, agreement does not exist on whether or how insurance cycles
could be moderated. The NAIC studies mentioned above noted that the
most likely primary causes of insurance cycles—changes in interest rates
and losses—were not subject to direct insurer or regulatory control.
32
In
addition, the studies also observed that underpricing by insurers during
soft markets likely increases the severity of premium rate increases during
the next hard market. But they did not agree on the question of using
regulation to prevent such swings in premium rates. Such regulation could
be difficult, for two reasons. First, because losses on medical malpractice
claims are volatile and difficult to predict, regulators could have difficulty
determining the appropriate level of premium rates to cover those losses.
In addition, restricting premium rate increases during hardening markets
could hurt insurer solvency and cause some insurers to withdraw from a
market with an already declining supply of insurance.
32
NAIC, Cycles and Crises.
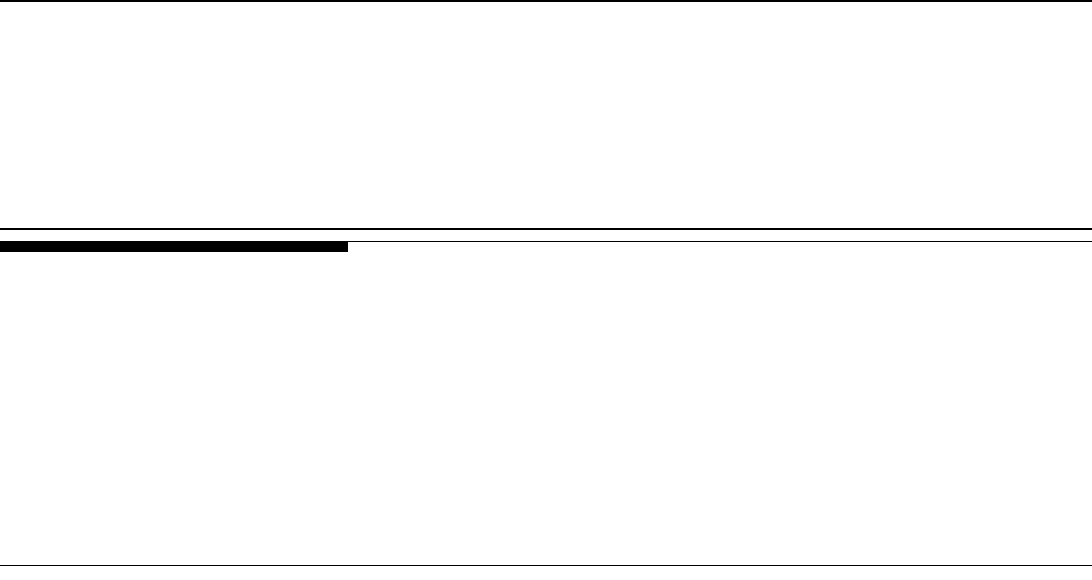
Page 37 GAO-03-702 Medical Malpractice Insurance
The Medical
Malpractice Insurance
Market Has Changed
since Previous Hard
Markets
The medical malpractice insurance market as a whole has changed
considerably since the hard markets of the mid-1970s and mid-1980s. These
changes have taken place over time and have been the result primarily of
actions insurers, health care providers, and state regulators have taken to
address rising premium rates. For example, insurers have moved from
occurrence-based to claims-made policies, physicians have formed mutual
nonprofit insurance companies that have come to dominate the market,
hospitals and groups of hospitals or physicians have increasingly chosen to
self-insure, and states have passed laws designed to slow the increase in
medical malpractice premium rates.
Beginning in the 1970s,
Insurers Began Selling
Claims-Made Rather Than
Occurrence-Based Policies
In order to more accurately predict losses and set premium rates, in the
mid-1970s most medical malpractice insurers began to change the type of
insurance policy they offered to physicians from occurrence based to
claims made. As we have noted, claims-made policies cover claims
reported during the year the policy is in effect, while occurrence-based
policies cover claims arising out of events that occurred during the year in
which the policy was in effect. Because claims-made policies cover only
reported claims, insurers can better estimate the payouts they will have to
make in the future. Occurrence-based policies do not provide such
certainty, because they leave insurers liable for claims related to the
incidents that occurred during a given year, including those not yet
reported to the insurer.
Claims-made policies can create difficulties for physicians needing or
wanting to change insurers, however, because the physician rather than the
insurer retains the risk of claims that have not yet been reported to the
insurer. However, most companies today offer separate policies providing
coverage for claims resulting from incidents that may have occurred but
were not reported before the physician switched companies. The vast
majority of policies in existence today are claims-made policies. In each of
the seven states we studied, for example, the leading insurer’s policies were
predominantly (if not exclusively) claims-made. This change in the type of
policy sold means that any changes to premium rates during future hard or
soft markets may differ from such changes in previous such markets.
Page 38 GAO-03-702 Medical Malpractice Insurance
Beginning in the Mid-1970s,
Groups of Physicians Joined
Together to Form Mutual
Insurance Companies
Faced with a surge in the frequency and severity of claims, many of the for-
profit insurers left the medical malpractice insurance market in the mid-
1970s. At the time, medical malpractice insurance was only a small portion
of most of the insurers’ overall business, so many companies chose simply
to discontinue their medical malpractice lines. However, this market
exodus led to a crisis of availability for physicians who wanted or needed
professional liability insurance. In response to this unmet demand,
physicians, often in connection with their state medical societies, joined
together to form physician-owned insurance companies. Initially,
physicians often needed to contribute capital in addition to their premiums
so that the companies would meet state capitalization requirements.
These new physician-owned insurance companies differed from existing
commercial carriers in several ways. First, the physician-owned companies
wrote predominantly claims-made policies, which, as previously discussed,
allowed the insurers to more accurately predict losses and set premium
rates. Second, in their initial years the new companies themselves enjoyed
significant short-term cost savings over commercial companies. Most
medical malpractice claims take several years to be resolved, and the
policies offered by the physician-owned companies covered only future
incidents of malpractice, so the companies had no existing claims that
needed to be paid immediately. The commercial companies’ occurrence-
based policies continued to provide coverage for malpractice that had
occurred before the new physician-owned companies began offering
policies. Thus the physician-owned companies would not incur the same
level of obligations as the existing carriers for several years, allowing the
physicians to pay an amount similar to the commercial premium and use
much of that money as capital contributions to surplus. Physician-owned
companies have several other advantages. To begin with, physician-owned
companies have a cost advantage because they do not need to provide
shareholders with profits. In addition, the physician-owned companies may
have some underwriting advantages over the for-profit entities, such as an
intimate knowledge of local doctors and hospitals and the legal customs
and climate. Finally, several insurers told us that these physician-owned
companies may have a different management philosophy than for-profit
companies, one that places greater emphasis on risk management and thus
lowers the incidence of claims. This philosophy may also extend to
defending claims more aggressively than traditional insurers.
Page 39 GAO-03-702 Medical Malpractice Insurance
Physician-owned and/or operated
33
insurance companies have grown to
dominate the medical malpractice insurance market, despite the fact that
most of them have not had the same access to the traditional capital
markets as for-profit insurers and therefore have had to build up their
surplus through premiums and capital contributions. Although several
physician-owned and/or operated insurance companies have expanded
their geographic presence and lines of insurance in the last decade, most of
these companies write insurance primarily in one state or a few states and
usually sell only medical malpractice liability insurance. Further, many of
the companies that had previously expanded have now retreated to their
original area and insurance line. As a result of this continuing change in the
composition of the medical malpractice insurance market, changes in
premium rates in the next soft market may be different from previous
markets, when commercial carriers dominated the market.
A Growing Number of
Individual Hospitals and
Hospital and Physician
Groups Have Begun Self-
Insuring
Over the past several years, an increasing number of individual hospitals
and consortia of hospitals and physicians have begun to self-insure
34
in a
variety of ways. Officials from the American Hospital Association
estimated that 40 percent of its member hospitals are now self-insured. In
states such as Florida that allow individual physicians to self-insure,
individual health care providers are also insuring themselves. Other
hospitals and groups of physicians are joining alternative risk-sharing
mechanisms, such as risk retention groups
35
or trusts.
36
Although some
hospitals and physicians have used these alternatives in the past, some
industry experts we spoke to said that the increasing movement to such
33
Some companies that were originally physician-owned have become publicly-held,
physician-operated insurers. While those insurers must now earn profits to satisfy
shareholders, and thus do not have all of the advantages that strictly physician-owned
insurers have, public, physician-operated insurers may have certain other advantages, such
as greater access to capital markets.
34
In general, self-insurance involves protecting against loss by setting aside funds to cover
potential claims rather than buying an insurance policy.
35
A risk retention group is a state-chartered liability insurance company owned by its
policyholders that can be formed as a stock or mutual insurance company. However, the
Risk Retention Act of 1986 preempts certain aspects of state laws regulating the activities of
risk retention groups.
36
A trust consists of segregated accounts of health care entities that simply estimate
liabilities and set aside funds to pay them. Some trusts are not required to have a surplus or
reserves.
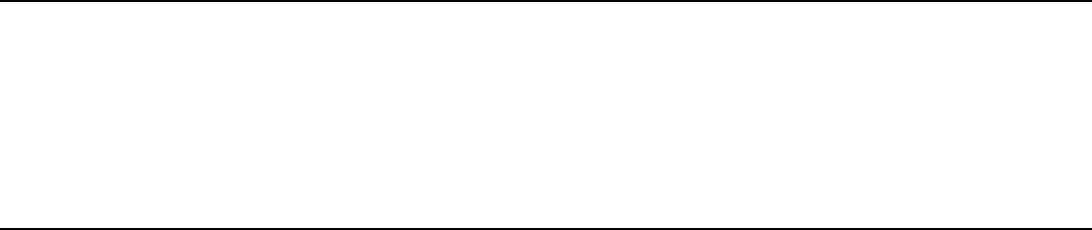
Page 40 GAO-03-702 Medical Malpractice Insurance
arrangements under the current market conditions indicates that some
health care providers are having difficulty obtaining insurance in the
traditional market.
While these arrangements could save money on the administrative costs of
insurance, they do not change the underlying costs of claims. Hospitals and
physicians insured through these arrangements often assume greater
financial responsibility for malpractice than they would under traditional
insurance arrangements and thus face a potentially greater risk of
insolvency. Although self-insured hospitals generally use excess loss
insurance for claims that exceed a certain amount, the hospitals must pay
the entire amount up to that threshold. Rather than a known number of
smaller payments on an insurance policy, the hospitals risk an unknown
number of potentially larger payments. And the threshold for excess loss
insurance is rising in a number of states. In Nevada, for example, some
hospitals’ excess loss insurance used to cover claim amounts in excess of
$1 million but now covers amounts above $2 million, leaving self-insured
hospitals with $1 million more exposure per claim. Self-insured physicians,
who have no other coverage for large losses, risk their personal assets with
every claim.
Hospitals and physicians are not the only ones more at risk under these
alternative arrangements. Claimants seeking compensation for their
injuries may have more difficulty obtaining payments from some of these
alternative entities and self-insured hospitals and physicians, for several
reasons. First, these entities and the self-insured are subject only to limited
public oversight, as state insurance departments do not regulate them.
Further, these entities do not participate in the state-run safety nets that
pay claims for insolvent insurance companies (state guaranty funds). Once
such a risk-sharing consortium fails, claimants may have no other recourse
but to try to enforce judgments against physicians personally. But enforcing
a judgment against a physician personally is generally more difficult than
obtaining payment under an insurance policy from a solvent insurance
company.
Page 41 GAO-03-702 Medical Malpractice Insurance
Data on these forms of insurance are sparse, so the extent to which
physicians and hospitals are using such arrangements is difficult to
measure. For example, NAIC and state insurance department data do not
include information on self-insurance or on most alternative risk-sharing
vehicles. In addition, one industry group has estimated that the information
available from A.M. Best, a recognized industry data source, accounts for
less than half the costs resulting from medical malpractice claims.
37
Like
the growth of physician-owned insurance companies, however, the growth
of such forms of insurance since the previous soft market may affect the
extent to which premium rates change in the next soft market.
All States Have Passed Laws
Designed to Reduce the
Growth of Medical
Malpractice Premium Rates
Since the medical malpractice crisis of the mid-1970s, all states have
enacted some change in their laws in order to reduce upward pressure on
medical malpractice premiums. Most of these changes are designed to
reduce insurers’ losses by limiting the number of claims filed, the size of
awards and settlements, and the time and costs associated with resolving
claims. Other changes are designed to help health care providers by more
directly controlling premium rates. Appendix II contains a more detailed
explanation of some of the types of legal changes that some states have
made, and appendix III contains more detail on the relevant laws in our
seven sample states.
Most of the state laws aimed at controlling premium rates attempt to
reduce insurer losses related to medical malpractice claims. Many of these
laws have similar provisions, the most controversial being the limitation, or
cap, on subjective, nonmonetary losses such as pain and suffering
(noneconomic damages). Several insurers and medical associations argue
that such a cap will help control losses on medical malpractice claims and
therefore moderate premium rate increases. But several trial lawyer and
consumer rights associations argue that such caps will limit consumers’
ability to collect appropriate compensation for their injuries and may not
reduce medical malpractice premium rates.
A cap on noneconomic damages may decrease insurers’ losses on claims by
limiting the overall amount paid out by insurance companies, especially
since noneconomic damages can be a substantial portion of losses on some
claims. Further, such a limit may also decrease the number of claims
37
Tillinghast-Towers Perrin, U.S. Tort Costs: 2002 Update, Trends and Findings on the
Costs of the U.S. Tort System (Atlanta, Ga.: February 2003).
Page 42 GAO-03-702 Medical Malpractice Insurance
brought against health care providers. Plaintiffs’ attorneys are usually paid
based on a percentage of what the claimant recovers, and according to
some trial attorneys we spoke with, attorneys may be less likely to
represent injured parties with minor economic damages if noneconomic
damages are limited.
Caps on noneconomic losses may have effects beyond reducing insurers’
costs. In theory, for example, after the frequency and severity of losses
have been reduced, insurers will decrease premium rates as well. Insurers
may also be better able to predict what they will have to pay out in
noneconomic damages because they can more easily estimate potential
losses, reducing the uncertainty that can give rise to premium rate
increases. Insurers reported that economic damages (generally medical
costs and lost wages), are more predictable than noneconomic damages,
which are generally meant to compensate for pain and suffering and thus
are very difficult to quantify.
In addition to attempting to decrease losses on medical malpractice claims,
two of our sample states have passed laws directly affecting premium rates
and insurance regulations. In a 1988 referendum, California passed
Proposition 103, which includes, among other things, a 20 percent rollback
of prices
38
for all property-casualty insurers (including medical malpractice
insurers), a 1-year moratorium on premium rate increases, and a provision
granting consumers the right to challenge any commercial insurance rate
increases greater than 15 percent. In 1995, Texas passed legislation that
required many insurance carriers, including medical malpractice insurers,
to reduce rates to a level deemed by the Texas Department of Insurance to
be acceptable, allowing for a reasonable profit. Texas passed the legislation
in conjunction with changes to Texas’ tort system. The legislators wanted
to avoid creating a windfall for insurers and believed that the companies
would not lower premium rates on their own until the impact of the
changes to the tort system could be actuarially determined.
Interested parties debate the impact these various measures may have had
on premium rates. However, a lack of comprehensive data on losses at the
insurance company level makes measuring the precise impact of the
measures impossible. As noted earlier, in the vast majority of cases,
38
The California Supreme Court allowed companies to decrease prices less than 20 percent
if a company could show that the rollback would make it impossible to earn a reasonable
profit.
Page 43 GAO-03-702 Medical Malpractice Insurance
existing data do not categorize losses on claims as economic or
noneconomic, so it is not possible to quantify the impact of a cap on
noneconomic damages on insurers’ losses. Similarly, it is not possible to
show exactly how much a cap would affect claim frequency or claims-
handling costs. In addition, while most claims are settled and caps apply
only to trial verdicts, some insurers and actuaries told us that limits on
damages would still have an indirect impact on settlements by limiting
potential damages should the claims go to trial. But given the limitations on
measuring the impact of caps on trial verdicts, an indirect impact would be
even more difficult to measure. Further, state laws differ dramatically, so
comparing their impact is difficult. For example, limitations on damages
can vary drastically in amount, type of damages covered, and how the
limitations apply. Some states have caps of $250,000 on noneconomic
damages, while other states have caps up to several times that amount.
Moreover, some dollar limits change over time—for instance, because they
are indexed to inflation—while others do not. Some states apply the cap to
all damages, including economic damages, and some apply the cap “per
occurrence” of malpractice. That is, the total amount collected by all
parties injured by an act of medical malpractice cannot exceed the cap,
regardless of how many physicians, hospitals, or other health care
providers may be partially liable for the injuries. In contrast, for example,
Nevada’s recently passed limitations on damages allow multiple plaintiffs
to collect the full limit from any number of responsible defendants.
The filing and resolution of medical malpractice claims is regulated, to a
great extent, by states’ tort and insurance laws. Changes to such laws can
thus have a great effect on both the frequency and severity of those claims,
which in turn can affect premium rates. Because many states have made
changes to these laws, it is difficult to predict the extent to which premium
rates might change in future markets.
Conclusions
Multiple factors have combined to increase medical malpractice premium
rates over the past several years, but losses on medical malpractice claims
appear to be the primary driver of increased premium rates in the long
term. Such losses are by far the largest component of insurer costs, and in
the long run, premium rates are set at a level designed to cover anticipated
costs. However, the year-to-year increase in premium rates can vary
substantially because of perceived future losses and a variety of other
factors, including investment returns and reinsurance rates. Moreover, the
market for medical malpractice insurance is not national, but depends on
the varying framework of insurance, legal, and health care structures
Page 44 GAO-03-702 Medical Malpractice Insurance
within each of the states. As a result, both the extent and the effects of
changes in losses and other insurance-related factors on premium rates
also vary by state.
While losses aggregated for the industry as a whole have shown a relatively
consistent upward trend over time, the loss experience of any single
company is likely to vary from year to year and to increase more rapidly in
some years than in others. At the same time, because of the long lag
between collecting premium income and paying on claims, premium rates
for the next year must be high enough to cover claims that will be reported
that year, the majority of which will be paid over the next 3 to 5 years. And
due to the volatility of the ultimate payouts on medical malpractice claims,
it is difficult for insurers to predict the amount of those payouts with great
certainty. As a result, changes in current losses can have large effects on
perceived or estimated future losses and consequently on premium rates,
because if insurers underestimate what will be needed to pay claims, they
risk not only future profits but potentially their solvency.
However, factors other than losses--such as changes in investment income
or the competitive environment--can also affect premium rate decisions in
the short run. These factors can either amplify or reduce the effect of
losses on premium rates. For example, high expected returns on
investment may legitimately permit insurers to price insurance below the
expected cost of paying claims. But incorrect projections of continuing
high returns could cause insurers to continue to hold prices down for too
long, even though underlying losses may be rising. When such factors
affect most or all medical malpractice insurers, the result appears as a
period of stable or falling premium rates or a period of sharply rising rates.
When they alternate, these periods may describe the soft and hard phases
of the medical malpractice insurance cycle.
Based on available data, as well as our discussions with insurance industry
participants, a variety of factors combined to explain the malpractice
insurance cycle that produced several years of relatively stable premium
rates in the 1990s followed by the severe premium rate increases of the past
few years. To begin with, insurer losses anticipated in the late 1980s did not
materialize as projected, so insurers went into the 1990s with reserves and
premium rates that proved to be higher than the actual losses they would
experience. At the same time, insurers began a decade of high investment
returns. This emerging profitability encouraged insurers to expand their
market share, as both the downward adjustment of loss reserves and high
investment returns increased insurers’ income. As a result, insurers were
Page 45 GAO-03-702 Medical Malpractice Insurance
generally able to keep premium rates flat or even reduce them, although
the medical malpractice market as a whole continued to experience
modestly increasing underlying losses throughout the decade. Finally, by
the mid- to late 1990s, as excess reserves were exhausted and investment
income fell below expectations, insurers’ profitability declined. Regulators
found that some insurers were insolvent, with insufficient reserves and
capital to pay future claims. In 2001, one of the two largest medical
malpractice insurers, which sold insurance in almost every state,
determined that medical malpractice was a line of insurance that was too
unpredictable to be profitable over the long term. Alternatively, some
companies decided that, at a minimum, they needed to reduce their size
and consolidate their markets. These actions, taken together, reduced the
availability of medical malpractice insurance, at least in some states,
further exacerbating the insurance crisis. As a result of all of these factors,
insurers continuing to sell medical malpractice insurance requested and
received large rate increases in many states. It remains to be seen whether
these increases will, as occurred in the 1980s, be found to have exceeded
those necessary to pay for future claims losses, thus contributing to the
beginning of the next insurance cycle.
While this explanation accounts for observed events in the market for
medical malpractice insurance, it does not provide answers to other
important questions about the market for medical malpractice insurance,
including an explanation of the causes of rising losses over time. The data
currently collected do not permit many of the analyses that would provide
answers to these questions. This lack of data is due, in part, to the nature of
NAIC’s and states’ regulatory reporting requirements for all lines of
insurance, which focus primarily on the information needed to evaluate a
company’s solvency. Most insurance regulators do not collect the data that
would allow analyses of the severity and frequency of medical malpractice
claims for individual insurer operations within specific states. Moreover,
insurers are generally not required to submit to NAIC or state regulators
data that would show how insurers losses are divided between settlements
and trial verdicts or between economic and noneconomic damages. Finally,
the increasing use of insurance or self-insurance mechanisms that are not
subject to state or NAIC reporting requirements further complicates a
complete analysis. While more complete insurance data would help
provide better answers to questions about how the medical malpractice
insurance market is working, other data would be equally important for
analyzing the underlying causes of rising malpractice losses and associated
costs. These data relate to factors outside the insurance industry, such as
policies, practices, and outcomes in both the medical and legal arenas.

Page 46 GAO-03-702 Medical Malpractice Insurance
However, collecting and analyzing such data were beyond the scope of this
report.
Matter for
Congressional
Consideration
Health care providers have suffered through three medical malpractice
insurance “crises” in the past 30 years. Each instance has generated
competing claims about the extent of the problem, the causes, and the
possible solutions. In each instance, a lack of necessary data has hindered
and continues to hinder the efforts of Congress, state regulators, and others
to carefully analyze the problem and the effectiveness of the solutions that
have been tried. Because of the potential for future crises, and in order to
facilitate the evaluation of legislative remedies put in place by various
levels of government, Congress may want to consider taking steps to
ensure that additional and better data are collected. Specifically, Congress
may want to consider encouraging NAIC and state insurance regulators to
identify the types of data that are necessary to properly evaluate the
medical malpractice insurance market—specifically, the frequency,
severity, and causes of losses—and begin collecting these data in a form
that would allow appropriate analysis. Included in this process would be an
analysis of the costs and benefits of collecting such data, as well as the
extent to which some segments of this market are not captured by current
data-gathering efforts. Such data could serve the interests of state and
federal governments and allow both to better understand the causes of
recurring crises in the medical malpractice insurance market and formulate
the most appropriate and effective solutions.
NAIC Comments and
Our Evaluation
NAIC’s Director of Research provided us with oral comments on a draft of
this report. The Director generally agreed with the report’s findings,
conclusions, and matter for congressional consideration. Specifically, the
Director agreed that the medical malpractice markets are not national in
nature and vary widely with regard to their insurance markets, regulatory
framework, legal environment, and health care structures. Furthermore,
the Director stated that the medical malpractice insurance industry has
shown an upward trend in losses over time and that this rise can be
attributed to a variety of causes that are difficult to measure or quantify.
The Director also said that he does not believe that excess profits by
insurers are in evidence.
The Director told us that NAIC is working on a study of the medical
malpractice marketplace that he hopes will be ready for distribution in the
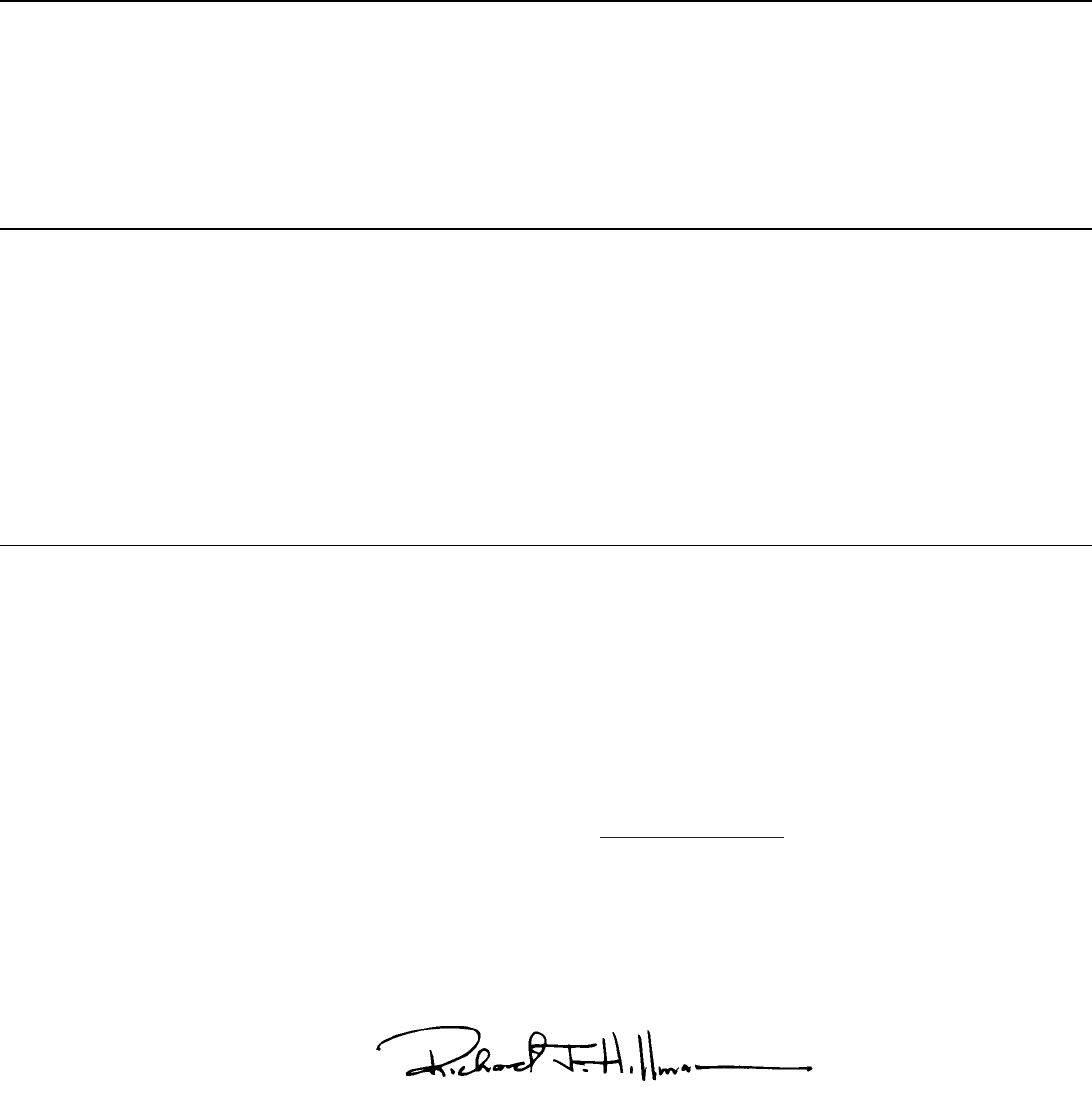
Page 47 GAO-03-702 Medical Malpractice Insurance
summer of 2003. The Director stated that NAIC, like GAO, had identified
many data limitations that make the study of this line of insurance difficult.
As a result, the Director generally agreed with our matter for congressional
consideration that Congress consider encouraging NAIC and state
regulators to identify and collect additional information that could be used
to properly evaluate the medical malpractice insurance market. The
Director stated that while such efforts would require some additional
resources, the costs would not be prohibitive and the efforts would provide
needed information. The Director also provided technical comments,
which we have incorporated into the report as appropriate.
As agreed with your offices, unless you publicly announce the contents of
this report earlier, we plan no further distribution until 30 days from the
report date. At that time, we will send copies of this report to the Chairmen
of the Senate Committee on Governmental Affairs and its Subcommittee on
Oversight of Government Management, the Federal Workforce, and the
District of Columbia; the Chairman of the House Committee on the
Judiciary; and the Chairman of the House Committee on Energy and
Commerce. We will also send copies of this report to other interested
congressional committees and members, and we will make copies available
to others on request. In addition, the report will be available at no charge
on the GAO Web site at http://www.gao.gov
.
If you or your staffs have any questions regarding this report, please
contact me or Lawrence Cluff at (202) 512-8678. Additional contributors
are acknowledged in appendix IV.
Richard J. Hillman
Director, Financial Markets and
Community Investment
Page 48 GAO-03-702 Medical Malpractice Insurance
List of Requesters
The Honorable Richard J. Durbin
Ranking Minority Member
Subcommittee on Oversight of Government Managment,
the Federal Workforce, and the District of Columbia
Committee on Governmental Affairs
United States Senate
The Honorable John Conyers, Jr.
Ranking Minority Member
Committee on the Judiciary
House of Representatives
The Honorable John D. Dingell
Ranking Minority Member
Committee on Energy and Commerce
House of Representatives
The Honorable Marion Berry
The Honorable Joseph M. Hoeffel
The Honorable Alan B. Mollohan
The Honorable Dennis Moore
The Honorable Nick J. Rahall II
The Honorable Max Sandlin
House of Representatives
Page 49 GAO-03-702 Medical Malpractice Insurance
Appendix I
AppendixesScope and Methodology Appendix I
Recognizing that the medical malpractice market can vary considerably
across states, we judgmentally selected a sample of seven states in order to
conduct a more in-depth review in each of those states. Except where
otherwise noted, our analyses were limited to these states. We selected our
sample so that we would have a mix of states based on the following
characteristics: extent of recent increases in premium rates, status as an
American Medical Association crisis state, presence of caps on
noneconomic damages, state population, and aggregate loss ratio for
medical malpractice insurers within the state. The states we selected were
California, Florida, Minnesota, Mississippi, Nevada, Pennsylvania, and
Texas. Within each state we spoke to one or both of the two largest and
currently active sellers of medical malpractice insurance, the state
insurance regulator, and the state association of trial attorneys. In six
states, we spoke to the state medical association, and in five states, we
spoke to the state hospital association. Due to time constraints, we did not
speak to the medical or hospital associations in Texas or the hospital
association in Florida. We used information obtained from these
organizations to help answer each of our objectives and, as outlined below,
also performed additional work for each objective.
To examine the extent of increases in medical malpractice insurance rates
for the largest insurers in our sample states, we reviewed annual survey
data on medical malpractice premium rates collected by a private data
collection company. While individual insurers determine whether to
respond to the survey, we believe the data to be representative for the three
medical specialties for which the company collects data—internal
medicine, general surgery, and obstetrics/gynecology—because of both the
number of insurers responding to the survey and the states represented by
them. The premium rates collected in the survey are base rates, which do
not reflect discounts or additional charges by insurers, so the actual
premium rates charged by insurers can vary from the premium rates
collected in the survey. We could not determine the extent to which the
actual premium rates charged varied from the base rates, but among the
insurers we spoke with, the actual premium rates charged in 2001 and 2002
ranged from about 50 to 100 percent of the base rates. We did not test the
reliability of the survey data.
To analyze the factors contributing to the premium rate increases in our
sample states and other states, we examined data from state insurance
regulators, the National Association of Insurance Commissioners (NAIC),
A.M. Best, the Securities and Exchange Commission, and the Physician
Insurers Association of America on insurers in our sample states as well as

Appendix I
Scope and Methodology
Page 50 GAO-03-702 Medical Malpractice Insurance
the medical malpractice insurance market as a whole. We did not verify the
reliability of these data. Where possible, we obtained data from 1975 to the
present. As noted earlier in this report, comprehensive, reliable data that
would have allowed us to quantify the effect of individual factors on
medical malpractice premium rates did not exist. We also reviewed
relevant academic studies and industry guidance. In addition, we spoke
with officials from the insurers and state insurance departments in our
sample states, as well as professional actuarial and insurance
organizations. To analyze factors that were likely to vary among states—
losses on medical malpractice claims, reinsurance rates, and competition
among insurers—we reviewed data for one or both of the two largest and
active medical malpractice insurers in our samples states. We also
reviewed aggregate data on losses for all insurers in each state as well as
the U.S. medical malpractice insurance market as a whole. To analyze
factors that were likely to be common among medical malpractice insurers
in all states—investment income and the presence of an insurance cycle—
we reviewed either A.M Best data for the 15 largest medical malpractice
insurers as of 2001 (whose combined market share nationally was
approximately 64.3 percent), or NAIC data for all medical malpractice
insurers reporting data to NAIC. Also as noted earlier in this report, data
and scope limitations prevented us from fully analyzing the factors behind
increased losses from medical malpractice claims.
To analyze how the national medical malpractice insurance market has
changed since previous periods of rising premium rates, we reviewed
studies published by NAIC; analyzed insurance industry data compiled by
NAIC and A.M. Best; reviewed tort laws across all states and state
insurance regulations; spoke with insurers and state insurance regulators
in our sample states; and spoke with officials from national professional
actuarial, insurance, legal, consumer rights, medical, and hospital
organizations.
We conducted our work from July 2002 through June 2003 in accordance
with generally accepted government auditing standards.
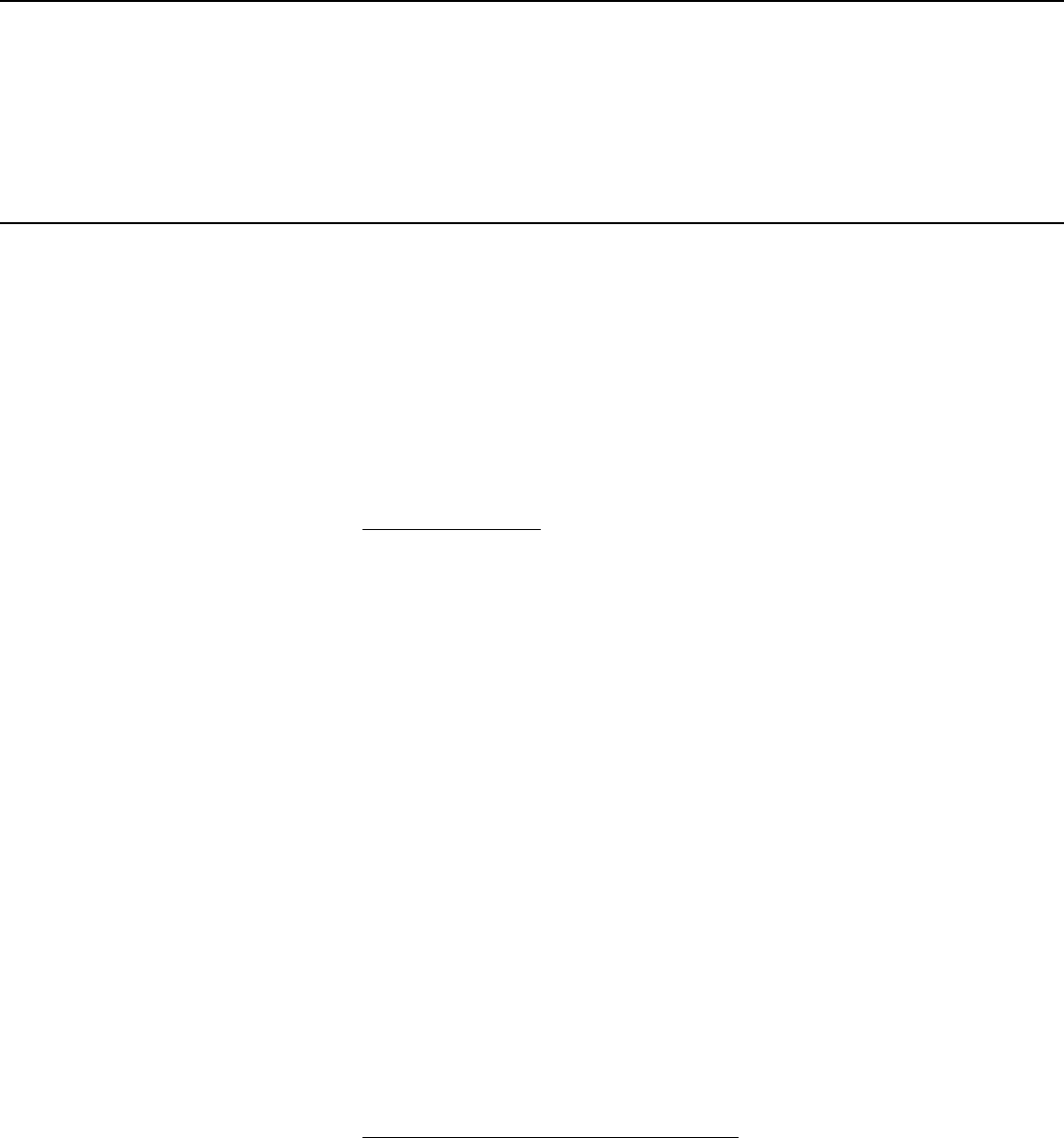
Page 51 GAO-03-702 Medical Malpractice Insurance
Appendix II
Legal Summary Appendix II
Each state’s tort laws generally govern the way in which medical
malpractice claims or lawsuits are resolved. As discussed in this report,
most state laws aimed at controlling premium rates attempt to reduce
insurer losses related to medical malpractice claims. Although these laws
take many different forms, they usually have at least some of the provisions
summarized in this appendix. State courts have dealt differently with these
kinds of provisions, and some states have found that some of these kinds of
provisions are unconstitutional. The provisions summarized in this
appendix are not the only ones that might impact the treatment of medical
malpractice claims in states’ tort systems.
Limits on Damages
. Damages in medical malpractice cases usually consist
of two categories, economic damages and noneconomic damages.
(Although punitive damages can be available in cases of gross negligence
and outrageous conduct of the health care provider, juries rarely award
punitive damages in medical malpractice cases.) Economic damages
generally consist of past and future monetary damages, such as lost wages
or medical expenses. Noneconomic damages generally consist of past and
future subjective, non-monetary loss, including pain, suffering, marital
losses, and anguish. Although some states have limits on the total amount
of damages recoverable in a medical malpractice suit, most states with
limits, as well as pending federal legislation, have emphasized a limit only
on noneconomic damages. As discussed in this report, limitations on
damages can vary drastically in amount, type of damages covered, and
application.
As mentioned in this report, limitations on damages can impact frequency
of lawsuits as well. Plaintiffs’ attorneys are usually paid based on a
percentage of what the claimant recovers, and according to some trial
attorneys we spoke to, attorneys may be less likely to represent an injured
party with minor economic damages if noneconomic damages are limited.
One consumer rights group told us that suits with limited economic
damages are typical in cases where the plaintiff is not working and does not
have substantial costs of future medical care.
Evidence of Collateral Source Payments
. At common law, or without any
legislative intervention, a plaintiff would be able to recover all damages
sustained from a liable defendant, even if the plaintiff were going to receive
money from other sources, called “collateral sources,” like health
insurance policies or Social Security. Some states have modified this
common law rule with statutes that allow defendants to show that the
claimant is going to receive funds from collateral sources that will
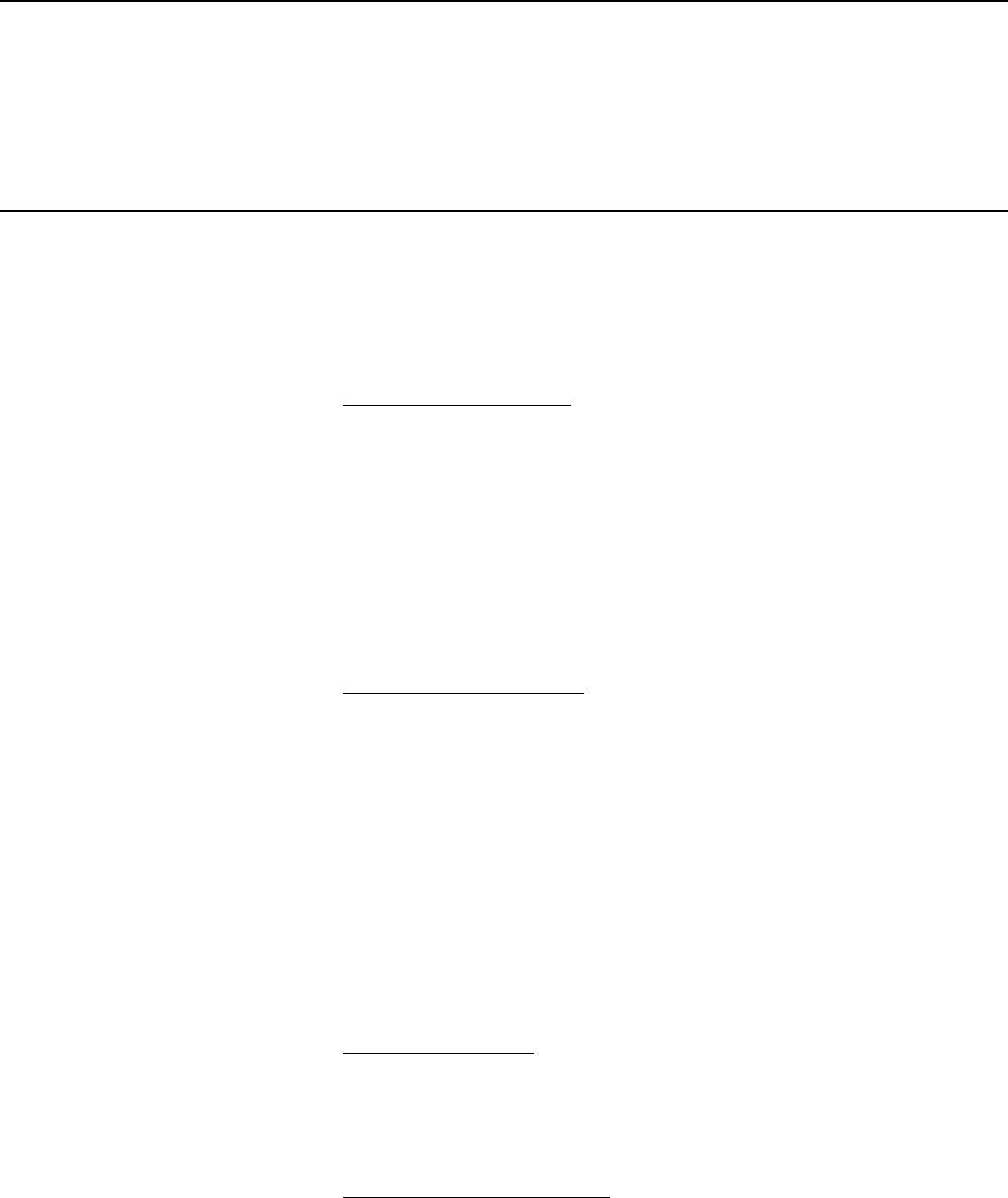
Appendix II
Legal Summary
Page 52 GAO-03-702 Medical Malpractice Insurance
compensate the claimant for damages he or she is attempting to collect
from the defendant. These statutes authorize, to various extents,
decreasing the defendant’s liability by the amount the claimant will receive
from other sources. In the state summaries in appendix III, if a state has not
modified the common law rule regarding collateral sources, the chart will
say “no modification.”
Joint and Several Liability
. Joint and several liability is the common law
rule that a plaintiff can collect the entire judgment from any liable
defendant, regardless of how much of the harm that defendant’s actions
caused. Some states have eliminated joint and several liability, making each
defendant responsible for only the amount or share of damage he or she
caused the plaintiff. Other states have eliminated joint and several liability
only for noneconomic damages. Some states have eliminated joint and
several liability for defendants responsible for less than a specified
percentage of the plaintiff’s harm; for example, if a defendant is less than 50
percent responsible, that defendant might need to pay only for that
percentage of the plaintiff’s damages.
Attorney Contingency Fees
. Most plaintiff attorneys are paid on a
contingency fee basis. A contingency fee is one in which the lawyer, instead
of charging an hourly fee for services, agrees to accept a percentage of the
recovery if the plaintiff wins or settles. Some states have laws that limit
attorney contingency fees. For example, in California a plaintiff’s attorney
can collect up to 40 percent of the first $50,000 recovered, 33 percent of the
next $50,000 recovered, 25 percent of the next $500,000 recovered, and 15
percent of any amount exceeding $600,000. Provisions that decrease
attorneys’ financial incentives to accept cases could decrease the number
of attorneys willing to take the cases. These limits were based on the belief
that they would lead to more selective screening by plaintiffs’ attorneys to
ensure that the claims filed had merit. In the state summaries in appendix
III, if a state does not have limits in place specifically for attorneys in
medical malpractice cases, the chart will say “no modification.”
Statute of Limitations
. The amount of time a plaintiff has to file a claim is
known as the “statute of limitations.” Some states have reduced their
statutes of limitations on medical malpractice claims. This decrease could
limit the number of cases filed by claimants. Special time requirements for
minors are not noted on the summaries in appendix III.
Periodic Payment of Damages
. Defendants traditionally pay damages in a
lump sum, even if they are being collected for future time periods, such as
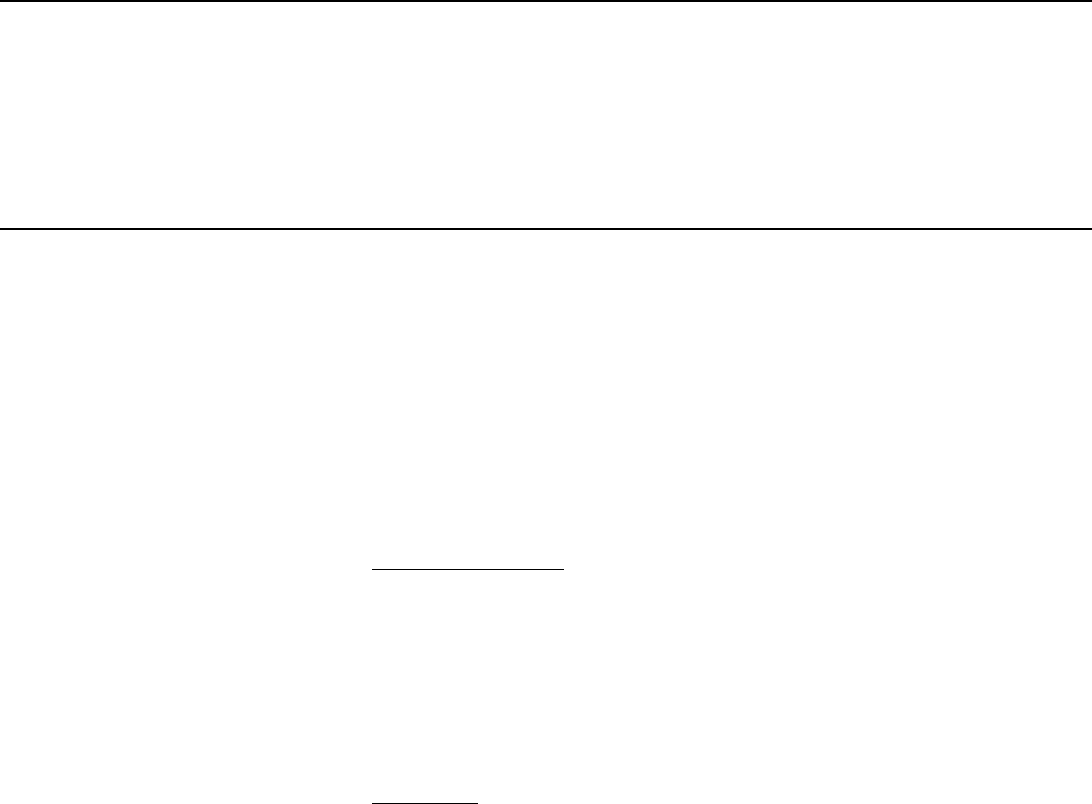
Appendix II
Legal Summary
Page 53 GAO-03-702 Medical Malpractice Insurance
future medical care or future lost wages. However, some states allow or
require certain damages to be paid over time, such as over the life of the
injured party or period of disability, either through the purchase of an
annuity or through self-funding by institutional defendants. Some insurers
we spoke with said that purchasing annuities can reduce insurers’ costs,
and that periodic payments better match damage payments to future
medical costs and lost earnings incurred by injured parties, assuring that
money will be available to the injured party in the future. A consumer rights
group we spoke with told us that, because periodic payments stop at the
death of an injured party, there may be unsatisfied medical bills at the time
of the injured party’s death.
Expert Certification
. Many states require that medical experts certify in
one way or another the validity of the claimant’s case. These statutes are
designed in part to keep cases without merit, also known as frivolous
cases, out of court. Expert certification requirements also have the
potential to get as many relevant facts out in the open as early as possible,
so that settlement discussions are fruitful and it becomes unnecessary to
take as many cases to trial, thus decreasing the claims-handling costs of the
case.
Arbitration
. Some states have enacted arbitration statutes that address
medical malpractice claims specifically. Some of these statutes require that
the arbitration agreement meets standards that are designed to alert the
patient to the fact that he is waiving a jury trial through the use of a specific
size of font, or by specifying the precise wording that must be contained in
the agreement. Although most courts have held that medical malpractice
claims can properly be submitted to arbitration, litigation involving the
arbitration statutes has involved issues such as whether the patient knew
he was waiving the right to a jury trial, whether the patient who agrees to
arbitration had appropriate bargaining strength, and whether third parties
have authority to bind others to arbitration.
By providing an option for arbitration, parties can avoid the larger expense
of taking claims to court. However, some industry experts said that these
arbitration provisions may not be binding and may result in the losing party
deciding to take the case to court in any event, so arbitration can simply
increase expenses without affecting the ultimate resolution of the dispute.
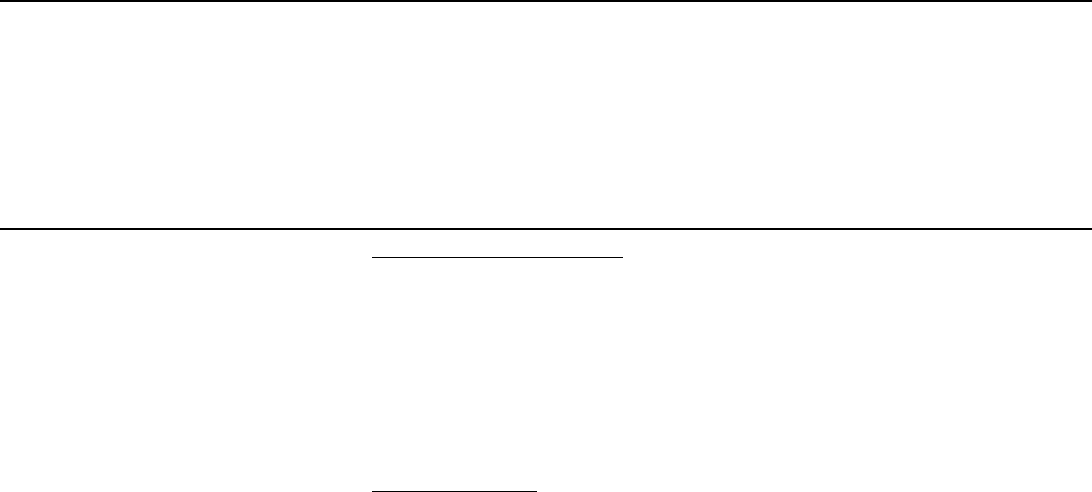
Appendix II
Legal Summary
Page 54 GAO-03-702 Medical Malpractice Insurance
Advanced Notice of Claim. Advanced-notice-of-claim provisions require
claimants to give defendants some period of time, 90 days for example,
prior to filing suit in court. Some insurers and plaintiffs’ attorneys we spoke
with said that this requirement aids plaintiffs and defendants in resolving
meritorious claims outside of the court system and allows plaintiffs’
attorneys to obtain relevant records to determine whether a case has merit.
However, another group we spoke to said that the advanced notice of claim
provision in that group’s state was ineffective.
Bad Faith Claims
. As mentioned in this report, some insurers we spoke
with told us that they can be liable for amounts beyond an insurance
policy’s limits, if the policyholder requests the insurer to settle with the
plaintiff for an amount equal to or less than the policy limit, and the insurer
takes the case to trial, loses, and a judgment is entered in an amount
greater than the policy limits. Industry experts we spoke to said that, under
those circumstances, the insurer could be liable for acting in “bad faith.” In
some states, like Nevada, this bad faith claim can be brought only by the
insured physician; that is, the physician can seek payment from the
insurance company if the physician has paid a plaintiff beyond a policy’s
limits. In contrast, in Florida, the plaintiff can sue a physician’s insurer
directly for the insurer’s alleged improper conduct in medical malpractice
cases. The difficulty of establishing that an insurer acted in bad faith varies
according to state law. Insurers in three of our study states—Texas,
California, and Florida—said that bad faith litigation was a substantial
issue in their states.
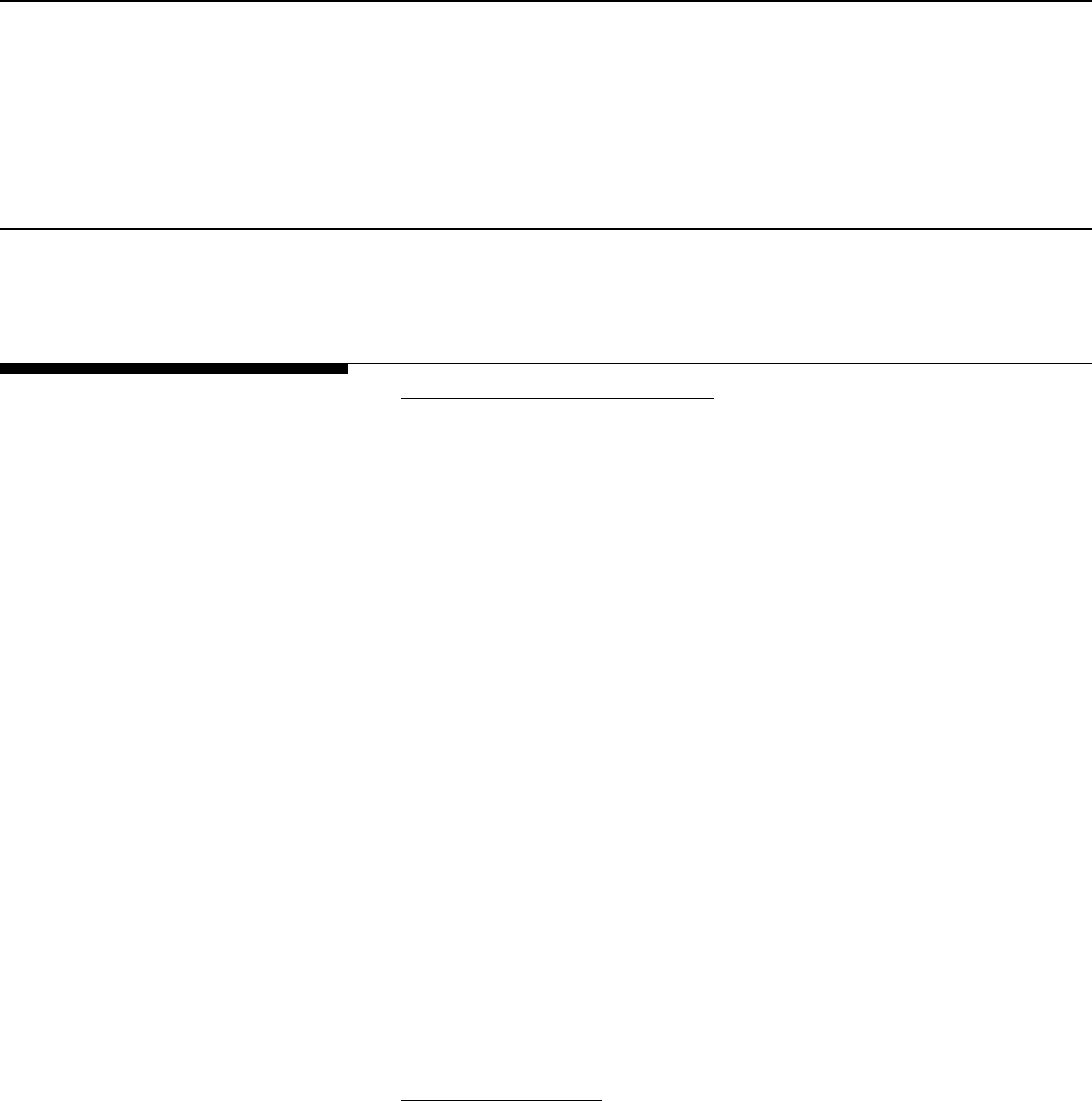
Page 55 GAO-03-702 Medical Malpractice Insurance
Appendix III
State Summaries Appendix III
This appendix describes the specific medical malpractice insurance
environment in each the seven sample states we evaluated for this report.
(See figs.10-16.)
Market Description
• Typical Coverage Type and Limit. This section summarizes the type of
medical malpractice insurance coverage typically issued in the state, as
well as the standard coverage limits of these policies. Coverage limits
can range from $100,000/$300,000 to up to $2 million /$6 million. The
lower number is the amount the insurer will pay per claim and the
higher number is the total the insurer will pay in aggregate for all claims
during a policy period. There are several types of insurance coverage
available.
• Occurrence-based insurance provides coverage for claims that arise
from incidents that occur during the time the insurance policy is in
force, even if the policy is not continued. Claims that arise from
incidents occurring during the policy period that are reported after
the policy’s cancellation date are still covered in the future.
• Claims-made insurance provides coverage for claims that arise from
incidents that occur and are reported during the time the insurance
policy is in force.
• Prior acts coverage is a supplement to a claims-made policy that can
be purchased from a new carrier when changing carriers. Prior acts
coverage covers incidents that occurred prior to the switch to a new
carrier but had not been previously reported.
• Tail coverage is an option available from a former carrier to continue
coverage for those dates that the claims-made coverage was in effect.
• Regional Differences
. This section notes any major regional differences
in premium rates quoted by insurers within the state using the base rate
for general surgery as a comparison. The Medical Liability Monitor
annually surveys providers of medical malpractice insurance to obtain
their premium base rates for three specialties: internal medicine,
obstetrics/gynecology, and general surgery. In the state summaries,
descriptions of regional differences in premium rates are based on
Medical Liability Monitor information.
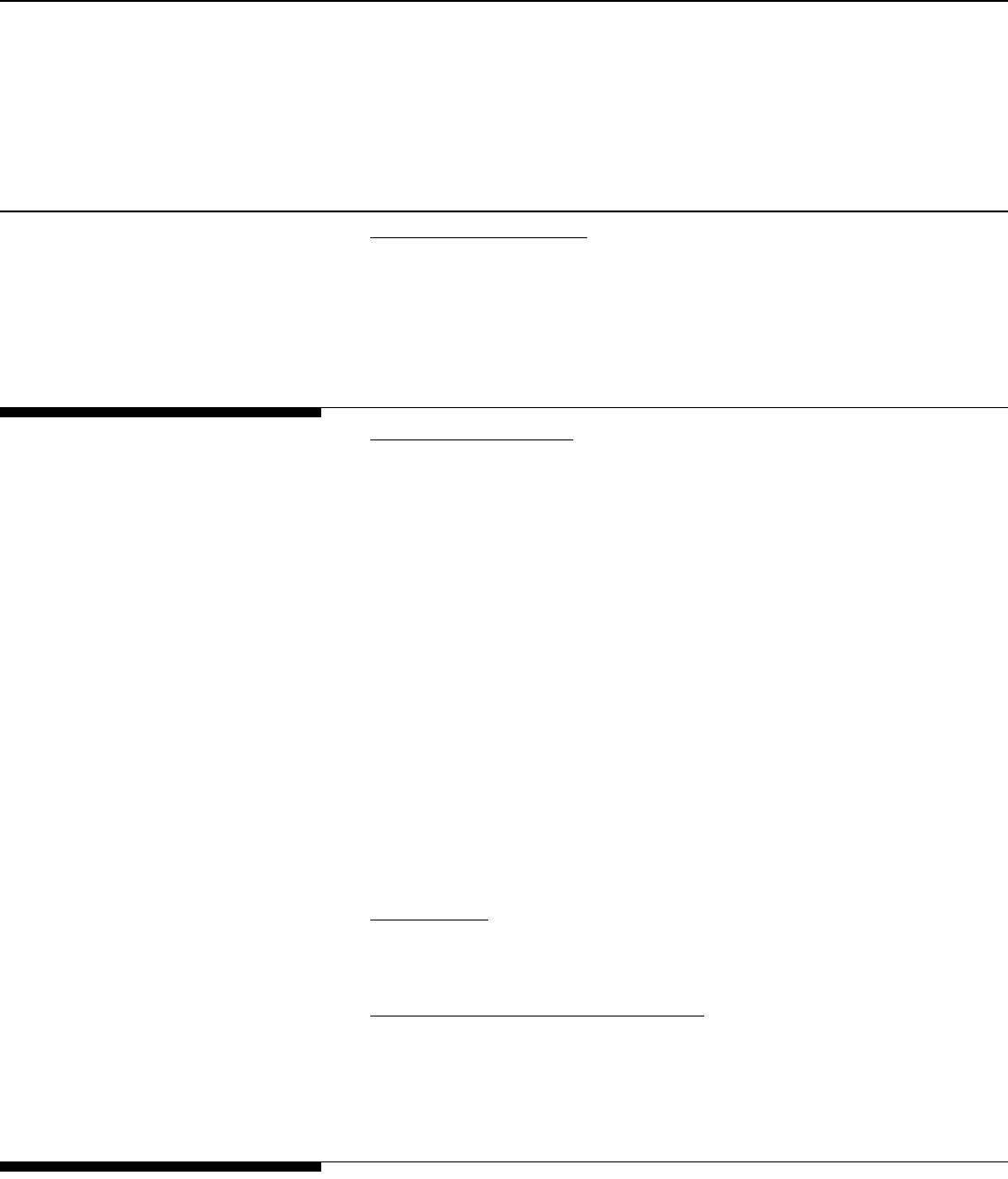
Appendix III
State Summaries
Page 56 GAO-03-702 Medical Malpractice Insurance
• Frequency and Severity. This section describes the extent to which
insurers and state regulators we spoke with believe frequency and
severity are changing in each state. Frequency is usually defined as the
number of claims per number of doctors, counting doctors in different
specialties as more or fewer doctors depending on the risk associated
with the specialty. Severity is the average loss to the insurer per claim.
Insurer Characteristics
and Market Share
• Insurer Characteristics. This section describes the various types of
insurers present in each of the states. In addition to traditional
commercial insurance companies, the following entities or
arrangements can provide liability protection:
• Physician insurer associations or physician mutuals are physician
owned and operated insurance companies that provide medical
liability insurance.
• Reciprocals are similar to mutuals, except that an attorney-in-fact
often manages the reciprocal.
• Risk retention groups are insurance companies owned by
policyholders. Risk retention groups are organized under federal
law—the Liability Risk Retention Act of 1986.
• Trusts are a form of self-insurance and consist of segregated
accounts of health care entities that estimate liabilities and set aside
funds to cover them.
• Market Share
. This section describes the medical malpractice market in
each of the states. Recent changes in the market are also noted in this
section.
• Joint Underwriting Association (JUA)
. This section details whether a
state has created a JUA and the extent of its use. A JUA is a state-
sponsored association of insurance companies formed with statutory
approval from the state for the express purpose of providing certain
insurance to the public.
Rate Regulation
This section describes the regulatory scheme employed by each state.
Statutory requirements generally provide that insurance rates be adequate,
Appendix III
State Summaries
Page 57 GAO-03-702 Medical Malpractice Insurance
not excessive, and not unfairly discriminatory. The degree of regulation of
medical malpractice insurance rates varies from state to state. States may
have “prior approval” requirements in which all rates must be filed with the
insurance department before use and must be either approved or
disapproved by the department of insurance. Other states have “file and
use” provisions in which the insurers must file their rates with the state’s
insurance department; however, the rates may be used without the
department’s prior approval.
State Tort Laws
This section identifies key components of each state’s efforts to address the
medical malpractice insurance situation by targeting ways in which
medical malpractice claims are processed through the court system. The
following legal provisions are summarized for each state:
• Limits on Damage Awards
• Collateral Source Rule
• Periodic Award Payments
• Pretrial Expert Certification
• Attorney Contingency Fees
• Joint and Several Liability
• Statute of Limitations
• Bad Faith Claims
Appendix II has a description of each of these provisions, in addition to
other provisions that are not summarized herein, but that might impact
medical malpractice claims. For the information on state provisions in
appendix III, we relied upon a summary of state tort laws compiled by the
National Conference of State Legislatures (NCSL) in October of 2002. We
independently reviewed selected sections of the NCSL summary for
accuracy, and supplemented the NCSL information with information from
interviews with industry officials. The state laws summarized herein might
have changed since the date of the NCSL publication. Additionally, as noted
in appendix II, the state tort laws summarized in this appendix are not the
Appendix III
State Summaries
Page 58 GAO-03-702 Medical Malpractice Insurance
only ones that might impact the treatment of medical malpractice claims in
states’ tort systems.
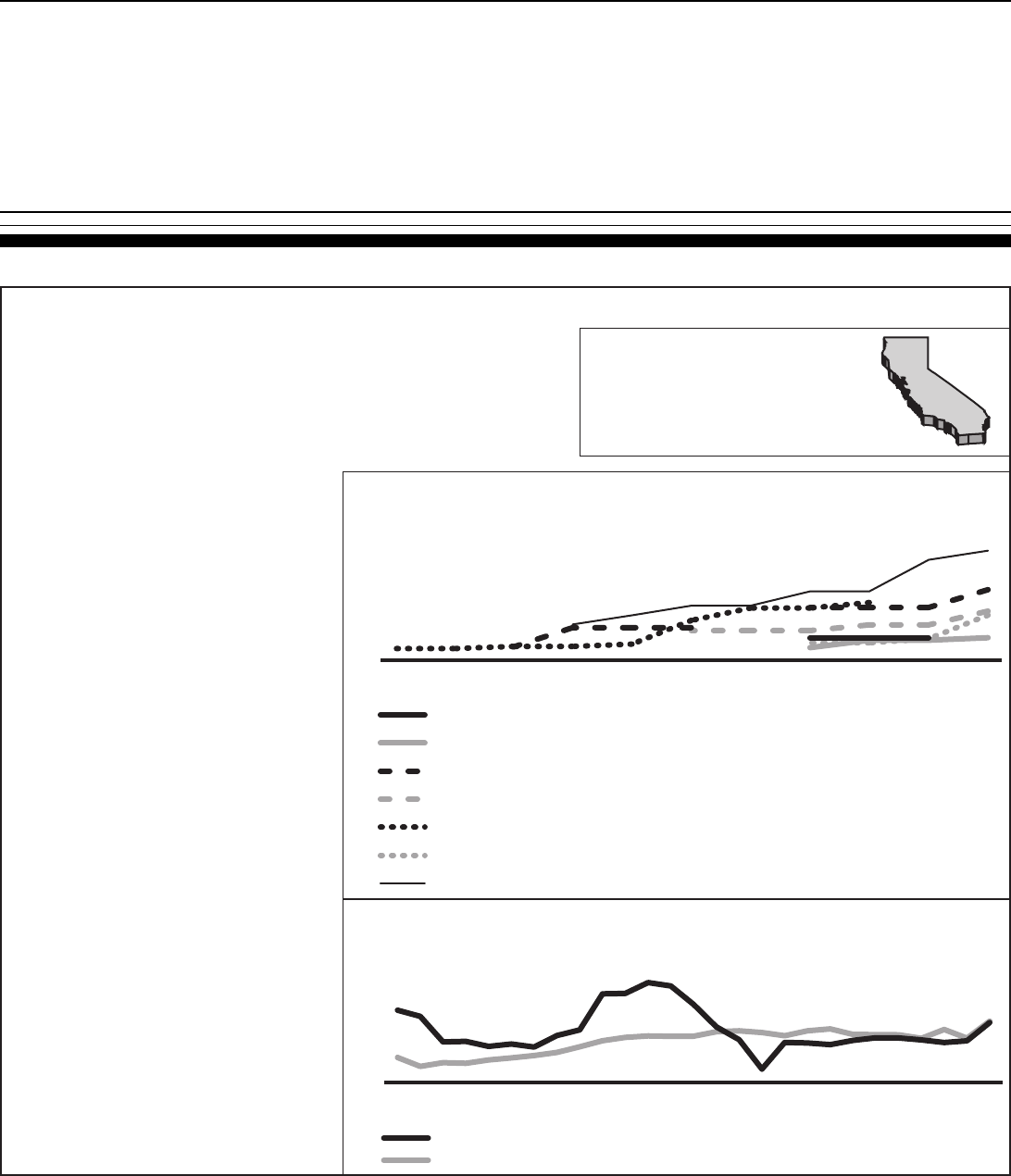
Appendix III
State Summaries
Page 59 GAO-03-702 Medical Malpractice Insurance
Figure 10: California
Sources: U.S. Census Bureau, 2000 (top box); GAO analysis of Medical Liability Monitor data (middle box); GAO analysis of A.M. Best data (bottom box).
CA
Market description:
Typical coverage type and limit-- Coverage is predominately claims-made. Typical policy limits
are $1 million per incident/$3 million cumulative for the policy year.
Regional differences-- Insurers generally divide California into two rating areas-northern and
southern California. Insurers typically reported higher rates for general surgery in southern
California counties.
Frequency and severity-- The California Department of Insurance (CDI) and insurers believe
severity is increasing in California and has led to increases in insurer losses.
Insurer characteristics and market share:
Insurer characteristics-- The California Medical
Association stated that most physicians in California
purchase medical malpractice coverage from
physician owned companies (Doctors Co., MIEC,
Norcal), commercial carriers (SCIPIE), or CAP/MPT,
a physician cooperative in which physicians assume
responsibility for the liabilities.
Market share-- Based on A.M. Best and NAIC data, the
companies with a 5% or more market share in
California (2001) were Norcal (21%), SCIPIE (13%),
Doctor's Co. (11%), CAP/MPT (9%), and Truck
Insurance Exchange (6%).
Rate regulation:
Prior to 1988 and the passage of Proposition 103,
California had an open filing system and had limited
interaction with its malpractice insurers. Proposition 103
requires prior approval of insurer rates. Additionally, if a
commercial carrier requests an increase of greater than
15 percent, the Commissioner of Insurance must grant a
public hearing upon request. At the time of passage,
insurers were also required to roll back their rates by
giving a refund to their clients.
State tort laws:
Limits on damage awards-- $250,000 limit on
noneconomic damages, applied per occurrence,
and not indexed for inflation.
Collateral source rule-- Discretionary offset for collateral
sources introduced at trial.
Periodic award payments-- Mandatory periodic payment
of future damages over $50,000 (upon request).
Pretrial expert certification-- Generally, no expert
certification is required for medical malpractice
cases in California.
Attorney contingency fees-- Limited to 40% of the first
$50,000, 33.3% of the next $50,000, and 25% of
the next $500,000, and 15% of any amount
exceeding $600,000.
Joint and several liability-- No joint and several liability
for noneconomic damages.
Statute of limitations-- Plaintiffs must file within one year
of discovery of injury or within three years of the
injury, whichever is first.
Bad faith claims-- Insurers consider this to be a
significant problem in California.
California
State specifics
Population: 33,871,648
Size (land area): 155,959 sq miles
Density: 217.2 pp/sq. mi
Premium Rates: General Surgery for Seven California Insurers
($1M/$3M mature claims-made coverage)
Direct Losses Paid Compared to Direct Losses Incurred
California 1975-2001
20
30
40
50
Southern California Phys. Ins. Ex. (SCPIE Indemnity Cos) in Riverside County
Northwest Physicians Mutual Insurance Co in the Los Angeles area
NORCAL Mutual Insurance Co.in Southern California
Medical Insurance Exchange of California (MIEC) in San Bernadino County
Doctors' Company in San Bernadino County
Cooperative of American Physicians, Inc. Mutual Protection Trust in Southern California
Clarendon Nat. Ins. Co. in San Bernadino County
20022001200019991998199719961995199419931992
Premium (dollars in thousands)
Direct losses paid
Direct losses incurred
0
200
400
600
800
20011999199719951993199119891987198519831981197919771975
Losses (in millions of 2001 dollars)
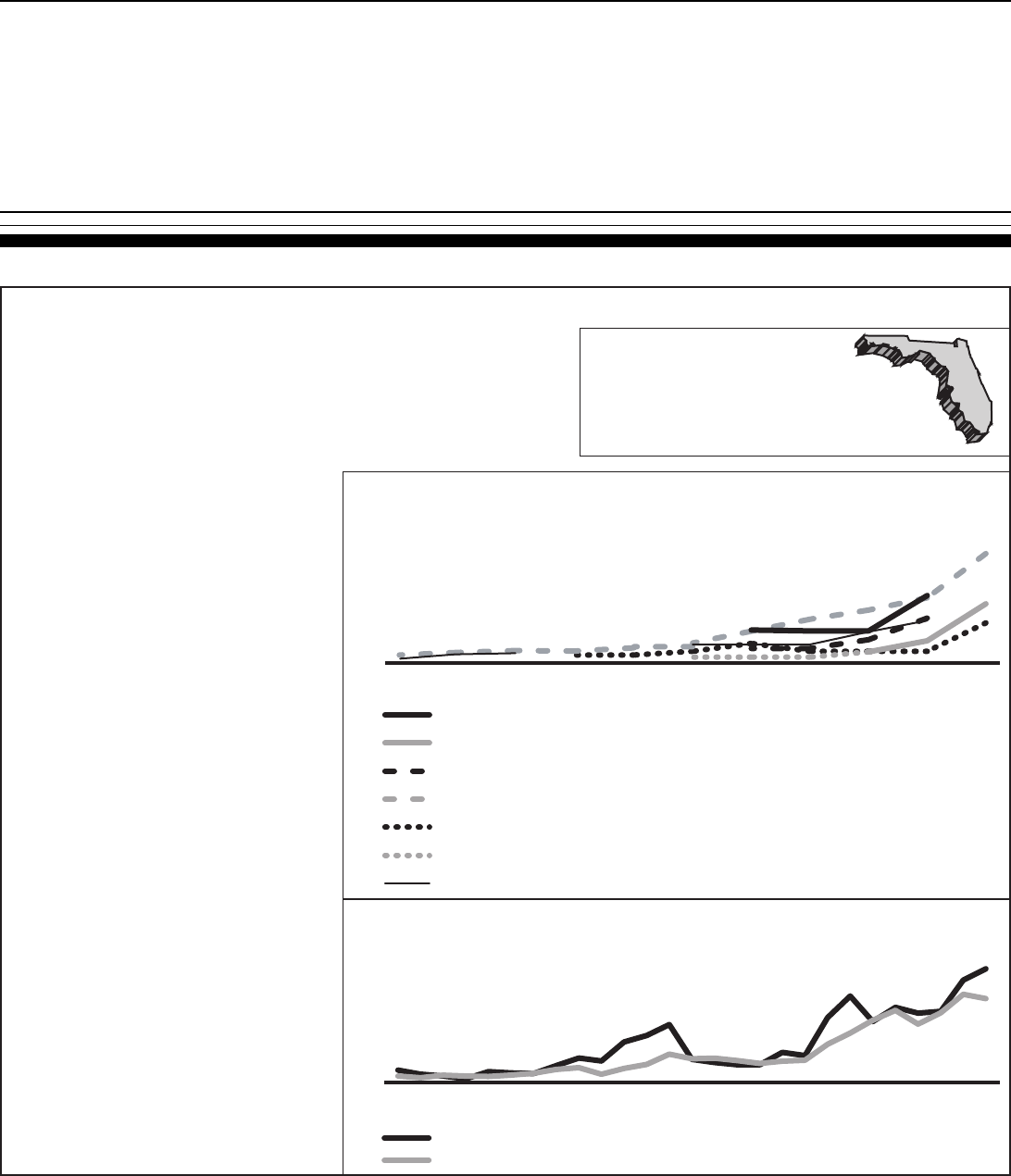
Appendix III
State Summaries
Page 60 GAO-03-702 Medical Malpractice Insurance
Figure 11: Florida
Sources: U.S. Census Bureau, 2000 (top box); GAO analysis of Medical Liability Monitor data (middle box); GAO analysis of A.M. Best data (bottom box).
Market description:
Typical coverage type and limit-- Many physicians are reducing the amount of coverage purchased. For
example, in 2002, First Professionals Insurance Company (FPIC) sold almost exclusively claims-made
policies with a $250,000 limit.
Regional differences-- Insurers typically reported higher rates for general surgery in Dade and Broward
Counties. According to the Florida Medical Association (FMA), Dade County has the highest premium
rates in the United States.
Frequency and severity-- FPIC believes claim frequency and severity have gone up significantly in the last
several years, with frequency responsible for the increased insurer losses.
Insurer characteristics and market share:
Insurer characteristics-- FMA stated that very few insurers in
Florida are currently physician owned. The state
Department of Insurance (DOI ) believes more hospitals
are self-insuring, more doctors are using the state JUA,
and many doctors are going without insurance. FPIC--
currently writing in 6 states--will only write in Florida
beginning in 2003.
Market share-- Based on A.M. Best and NAIC data, the
companies with a 5% or more market share in Florida
(2001) were FPIC (17%), Health Care Indemnity Inc.
(14%), Pronational Insurance Company (9%), and Truck
Insurance Exchange (5.4%).
Joint Underwriting Association-- Florida has a JUA, which
acts as an insurer of last resort. The number of health
care providers using the JUA has increased from around
20 in 2000 to 400 in 2001
Rate regulation:
Florida is a use and file state. There is no allowable deviation
from the approved rate filing, which must include all possible
adjustments to the base rate.
State tort laws:
Limits on damage awards-- Where parties agree to binding
arbitration (requires defendant admit fault), noneconomic
damages are limited to $250,000; where plaintiff refuses
to arbitrate, noneconomic damages are limited to
$350,000. The limits are applied per plaintiff.
Collateral source rule-- Mandatory offset of collateral sources
by court, unless sources have subrogation rights.
Periodic award payments-- Periodic payment of future
damages allowed if damages exceed $250,000.
Pretrial expert certification-- Verified medical expert opinion
required at the time of notice of intent to initiate litigation.
Attorney contingency fees-- Separate sliding scales for cases
settling at various points of the judicial process.
Joint and several liability-- Sliding scale for defendant's
responsibility, depending on whether plaintiff had any
responsibility for harm and how responsible the
defendant is for the harm. For example, if the plaintiff is
not at fault and the defendant is less than 10%
responsible, the defendant need not pay more than the
percentage for which defendant was found responsible.
Statute of limitations-- Plaintiff must file within two years of
occurrence or discovery, but not more than four years
from occurrence.
Bad faith claims-- The Florida Department of Insurance said
that bad faith lawsuits are having a significant impact on
insurer losses and, therefore, on premium rates.
Florida
State specifics
Population: 15,982,378
Size (land area): 53,927 sq miles
Density: 296.4 pp/sq. mi
Premium Rates: General Surgery for Eight Florida Insurers
($1M/$3M mature claims-made coverage)
Direct Losses Paid Compared to Direct Losses Incurred
Florida 1975-2001
Direct losses paid
Direct losses incurred
FL
ProNational Ins. Co. in Dade County
Michigan Physicians Mutual Liability Co. (MICOA) in Dade County
Medical Assurance in Dade County
First Professionals or Florida Physicians Insurance Co. (FPIC) in Dade County
Clarendon Nat. Ins. Co.in Dade County
American Physicians Assurance Corp. (AP Capital) in Dade County
American Healthcare Indemnity Co. (SCPIE Cos.) in Dade County
Losses (in millions of 2001 dollars)
0
200
400
600
800
20011999199719951993199119891987198519831981197919771975
Premium (dollars in thousands)
50
100
150
200
20022001200019991998199719961995199419931992
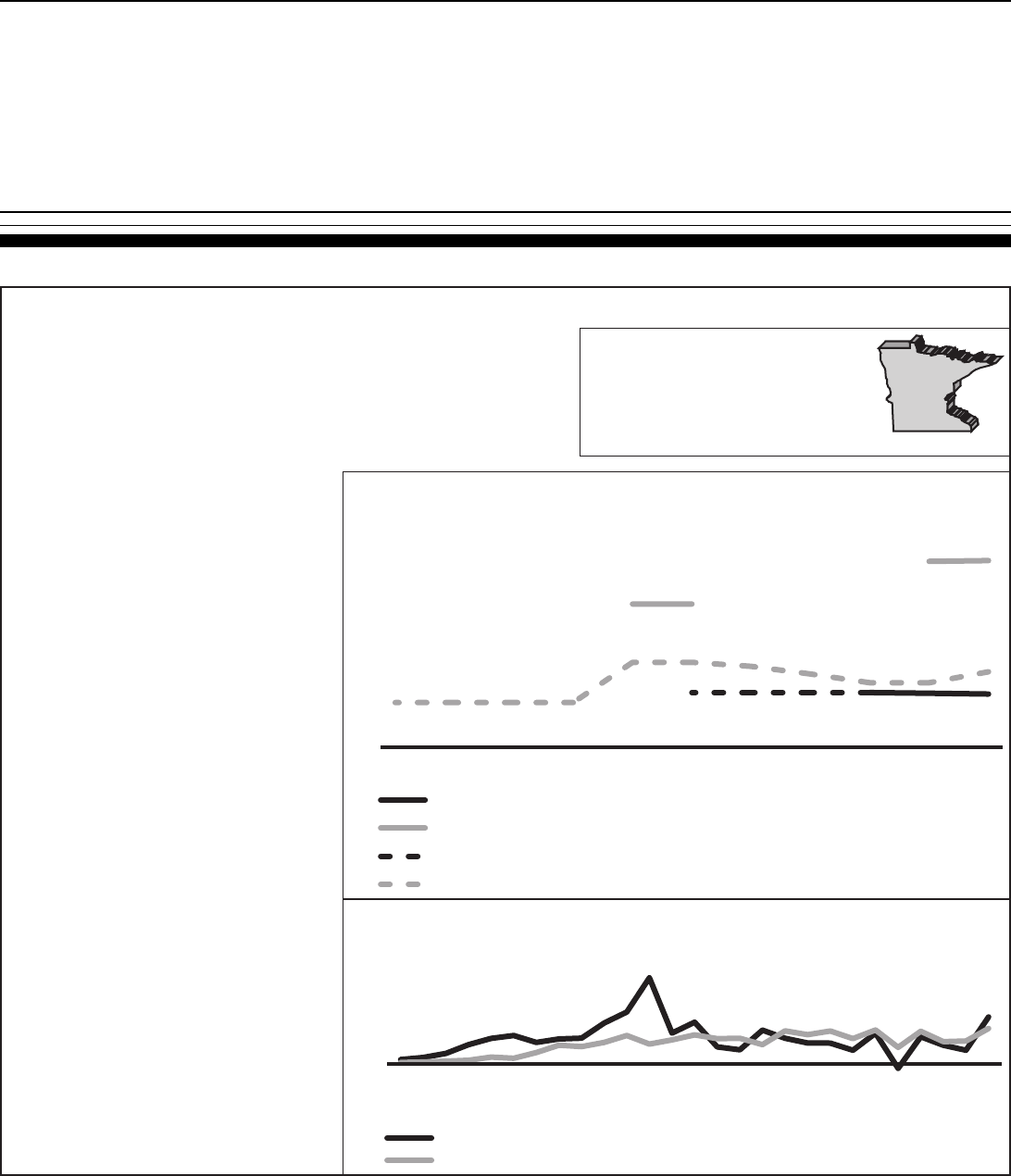
Appendix III
State Summaries
Page 61 GAO-03-702 Medical Malpractice Insurance
Figure 12: Minnesota
Sources: U.S. Census Bureau, 2000 (top box); GAO analysis of Medical Liability Monitor data (middle box); GAO analysis of A.M. Best data (bottom box).
Market description:
Typical coverage type and limit-- Coverage is predominately claims-made. Typical policy limits are $1
million per incident/$3 million cumulative for the policy year, although some physicians purchase
$2 million /$4 million coverage.
Regional differences-- Insurers typically treat Minnesota as single rating area.
Frequency and severity-- According to the Minnesota Medical Association (MMA), there has been a slight
increase in the severity of claims in the past several years and no observed increase in frequency.
Insurer characteristics and market share:
Market share-- According to A.M. Best, the companies with
a 5% or more market share in Minnesota in 2001 were
Midwest Medical Insurance Company (51%) and St. Paul
(26%). The St. Paul Companies recently discontinued
their medical malpractice insurance line in Minnesota.
Midwest Medical Insurance Company is now the leading
medical malpractice insurer in Minnesota; it grew over
50% in the last two years.
Joint Underwriting Association-- In Minnesota, the JUA is
considered the insurer of last resort. As of 1/2002, the
JUA had 8 policies but by 10/2002 it had 168 policies,
mostly for nursing homes.
Rate regulation:
The state regulatory body--Minnesota Department of
Commerce--emphasizes the market itself as the most
effective regulator of premium rates in the state. Minnesota
has a file and use system. In 2001, Minnesota began to
allow a "speed to market" filing procedure for companies that
meet certain stability and history requirements.
State tort laws:
Limits on damage awards-- No limit on economic or
noneconomic damages.
Collateral source rule-- Minnesota requires a mandatory
offset of collateral sources by court if defendant
introduces evidence of payments made to plaintiff.
Periodic award payments-- Allows discretionary periodic
payment of future damages if damages exceed $100,000.
Pretrial expert certification-- With the initial filing, plaintiff's
expert must certify defendant deviated from the
applicable standard of care and that deviation caused
plaintiff's injuries. After 180 days, expected trial expert
must certify as to the substance of facts and opinions to
which expert is expected to testify, and grounds to
support those opinions.
Attorney contingency fees-- No modification.
Joint and several liability-- Defendant liable only for up to four
times defendant's share of damages if less than 15%
responsible for harm; if more than 15% responsible,
defendant liable for entire amount of damages. After
August 1, 2003, defendent liable for proportioned share
of damages, if less than 50% responsible for harm; if
more than 50% responsible, defendant liable for entire
amount of damages.
Statute of limitations-- Plaintiff must file within two years of
occurrence of malpractice or termination of treatment.
Bad faith claims-- Insurer and medical society did not say
these cases were an issue in Minnesota.
Minnesota
State specifics
Population: 4,919,479
Size (land area): 79,610 sq miles
Density: 61.8 pp/sq. mi
Premium Rates: General Surgery for Four Minnesota Insurers
($1M/$3M mature claims-made coverage)
Direct Losses Paid Compared to Direct Losses Incurred
Minnesota 1975-2001
Direct losses paid
Direct losses incurred
Losses (in millions of 2001 dollars)
MN
Midwest Medical Insurance Co. (MMIC aka Midwest Mutual)
Michigan Physicians Mutual Liability Co. (MICOA)
Doctors' Company
American Physicians Assurance Corp. (AP Capital)
Premium (dollars in thousands)
5
10
15
20
20022001200019991998199719961995199419931992
-20
0
20
40
60
80
100
120
20011999199719951993199119891987198519831981197919771975
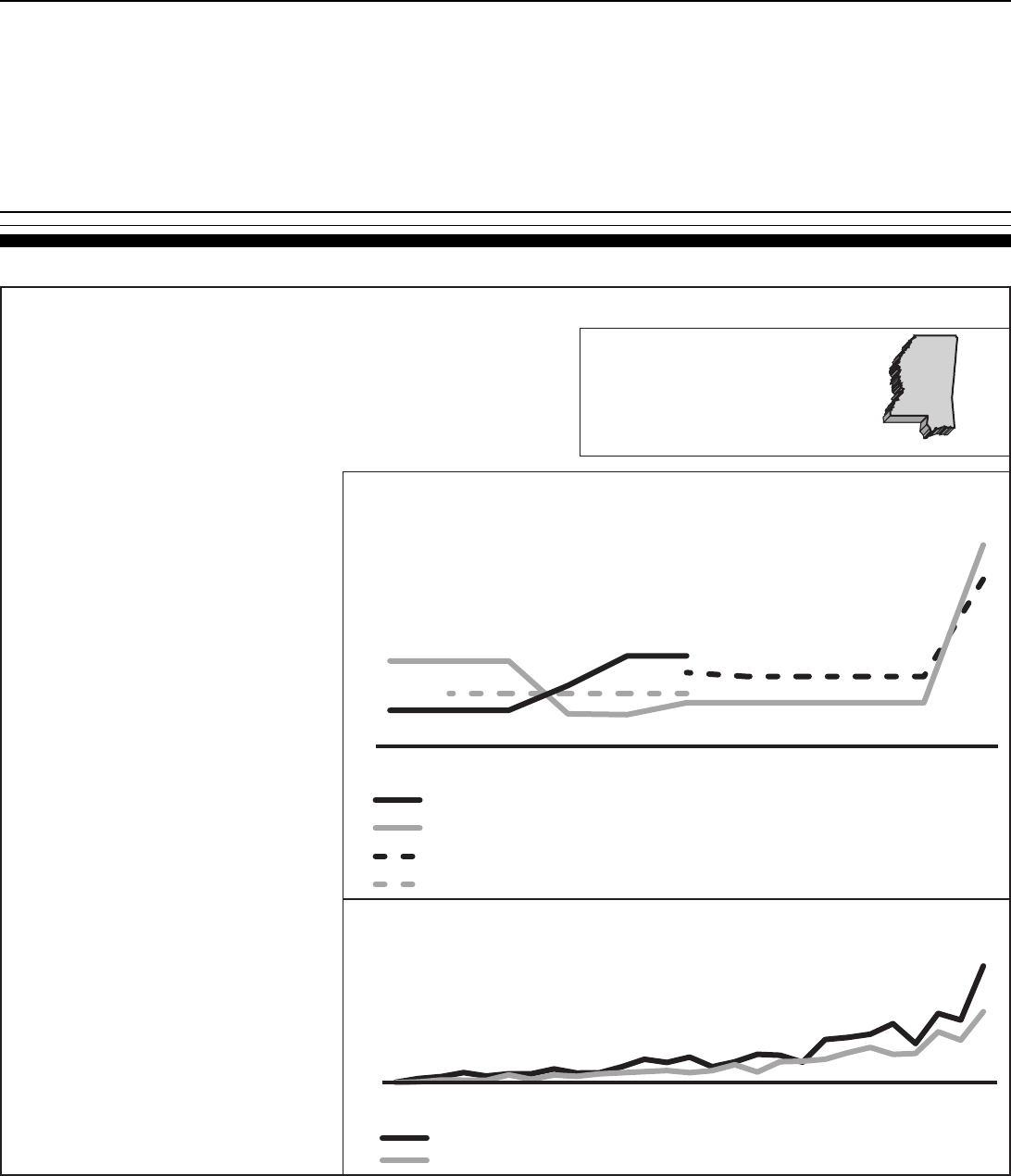
Appendix III
State Summaries
Page 62 GAO-03-702 Medical Malpractice Insurance
Figure 13: Mississippi
Sources: U.S. Census Bureau, 2000 (top box); GAO analysis of Medical Liability Monitor data (middle box); GAO analysis of A.M. Best data (bottom box).
Market description:
Typical coverage type and limit-- The Mississippi Department of Insurance (DOI) stated that insurance in
the state is typically claims made.
Regional differences-- Insurers typically treat Mississippi as a single rating area.
Frequency and severity-- The DOI and Medical Assurance Company of Mississippi (MACM) believe claim
severity has grown significantly and has led to increased insurer losses.
Insurer characteristics and market share:
Insurer characteristics-- According to a 2003 DOI survey,
some physicians are moving from the admitted market to
the surplus market. DOI stated that some physicians are
going without formal insurance right now and hospitals
might be moving to form risk retention groups or self-
insure, but that captives are not allowed under state law.
Market share-- Based on A.M. Best and NAIC data, the
companies with a 5% or more market share in
Mississippi (2001) were MACM (34%), Reciprocal of
America (21%), St. Paul Companies (10%), Doctors
Insurance Reciprocal (8%), and the Doctor's Company
(6%). DOI stated that MACM is the largest writer in
Mississippi with an estimated market share of 60
percent. Most licensed companies, including MACM are
at no growth. Several companies--St. Paul, Reciprocal of
America, ProAssurance--have pulled out of the market or
are reducing exposure.
Joint Underwriting Association-- DOI is currently
investigating whether a JUA would be worthwhile.
Rate regulation:
The DOI stated that most medical malpractice insurance in
Mississippi is presently being written in the non-admitted
market (surplus lines), which is not rate or form regulated.
DOI does not regulate the rates or forms of MACM because
it is a non-profit, mutual insurance corporation.
State tort laws:
Limits on damage awards-- $500,000 limit on noneconomic
damages, increasing to $750,000 on July 1, 2011 and
$1,000,000 on July 1, 2017; limit does not apply in
disfigurement cases or at the judge's discretion.
Collateral source rule-- No modification.
Periodic award payments-- No provisions for such payments.
Pretrial expert certification-- Plaintiff's attorney must file a
certificate of expert consultation, unless an exception to
that general rule applies.
Attorney contingency fees-- No limitation.
Joint and several liability-- There is no joint and several
liability for noneconomic damages in medical malpractice
cases. For economic damages, Mississippi has a sliding
scale, where defendants less than 30% responsible pay
only their proportionate share, but defendants over 30%
responsible pay up to 50% of economic damages.
Statute of limitations-- Plaintiff must file within two years of
the malpractice of reasonable discovery of malpractice
or seven years of the act.
Bad faith claims-- The insurer we spoke to said that it has
not yet been sued for bad faith.
Mississippi
State specifics
Population: 2,844,658
Size (land area): 46,907 sq miles
Density: 60.6 pp/sq. mi
Premium Rates: General Surgery for Four Mississippi Insurers
($1M/$3M mature claims-made coverage)
Direct Losses Paid Compared to Direct Losses Incurred
Mississippi 1975-2001
Direct losses paid
Direct losses incurred
MS
P-I-E Mutual Ins. Co.
Medical Assurance of West Virginia (Part of ProAssurance)
Medical Assurance Co of Miss (MACM)
Doctors' Company
Premium (dollars in thousands)
10
15
20
25
30
35
20022001200019991998199719961995199419931992
Losses (in millions of 2001 dollars)
0
40
80
120
20011999199719951993199119891987198519831981197919771975
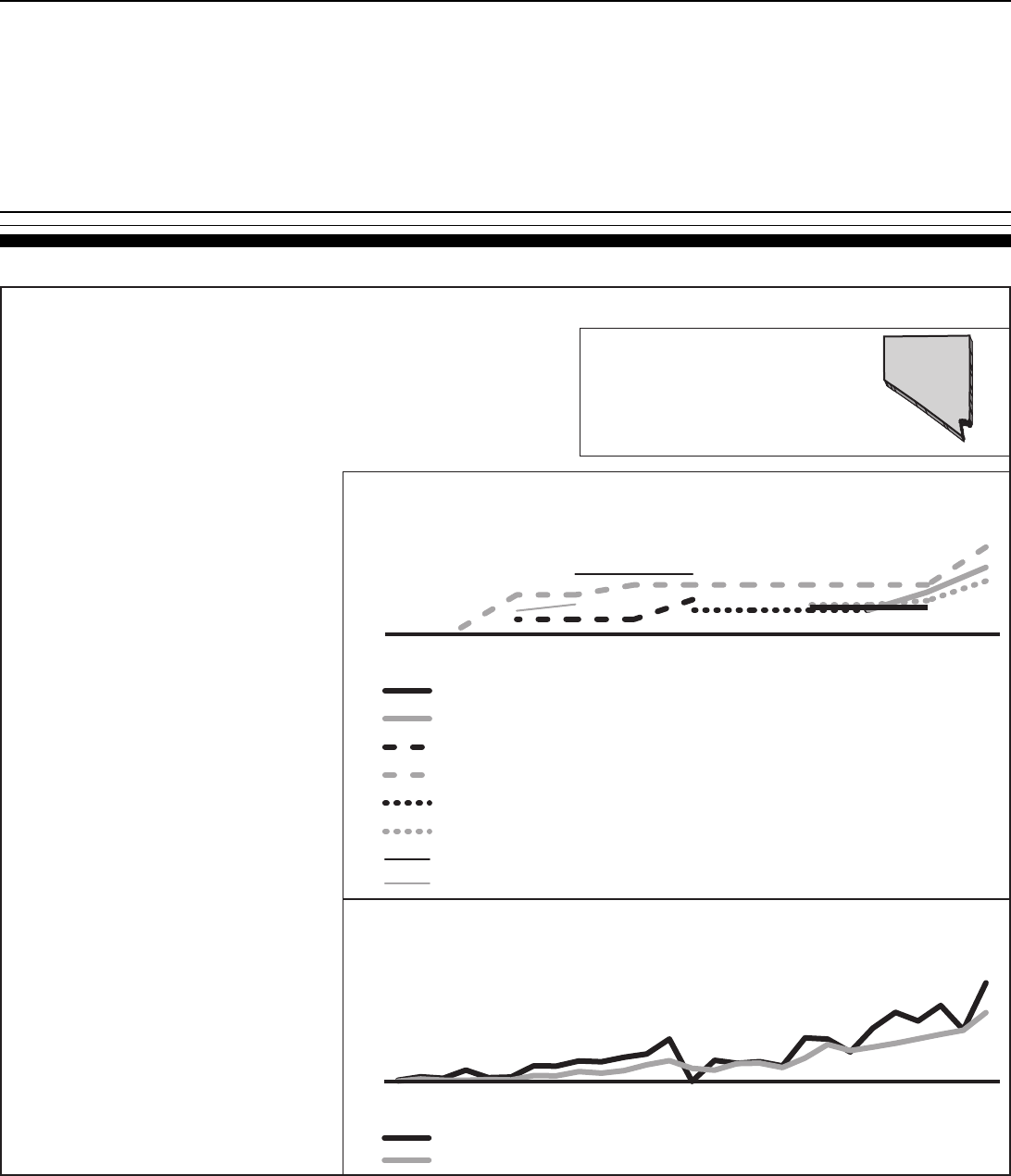
Appendix III
State Summaries
Page 63 GAO-03-702 Medical Malpractice Insurance
Figure 14: Nevada
Sources: U.S. Census Bureau, 2000 (top box); GAO analysis of Medical Liability Monitor data (middle box); GAO analysis of A.M. Best data (bottom box).
Market description:
Typical coverage type and limit-- Most policies are claims-made, with the exception of a few physicians in
low-risk specialties. In Nevada, most physicians are required to have $1 million/$3 million coverage.
Frequency and severity-- The State Department of Insurance (DOI) has closed-claim data indicating that
frequency has increased over the past several years. The DOI believes this increase in severity is one
of the main reasons insurer losses are increasing in Nevada. The Nevada State Medical Association
does not believe frequency is increasing in Nevada.
Regional differences-- Insurers reporting to the Medical Liability Monitor survey typically charge higher
premiums for general surgery in Las Vegas and Clark County.
Insurer characteristics and market composition:
Insurer characteristics-- In 2002, the state created Medical
Liability Association of Nevada (MLAN). Although initially
organized by the Insurance Commissioner, it will be an
independent insurer and has the ability to convert to a
mutual in the future. Also in 2002, Nevada Mutual
Insurance Company (NMIC), a physician owned
company, was formed and entered the market.
Market share-- Based on A.M. Best and NAIC data, the
companies with a 5% or more market share in Nevada
(2001) were St. Paul (32%), Health Care Indemnity Inc.
(13%), the Doctors Company (9%), Physician Insurance
Company of Wisconsin (6%), and Chicago Insurance
Company (6%). St. Paul acquired Nevada Medical
Liability Insurance (NMLI) in the mid 1990s, and captured
a majority market share in Nevada. In December 2001,
St. Paul announced it would be exiting the medical
malpractice business.
Rate regulation:
The DOI requires prior approval of rates.
State tort laws:
Limits on damage awards-- $350,000 limit on noneconomic
damages, with exception for cases of gross malpractice
or special circumstances. Cap is applied per plaintiff and
per defendant.
Collateral source rule-- Courts allow offsets in damages
against health care providers in the amount received
from a collateral source, including any prior payment by
the defendant health care provider.
Periodic award payments-- Claimant may elect to receive
award for future damages in a lump sum reduced to
present value, if approved by the court, or by an annuity.
Pretrial expert certification-- Expert certification required to
support allegations; expert must practice or have
practiced in area similar to practice related to alleged
malpractice.
Attorney contingency fees-- No modification.
Joint and several liability-- There is no joint and several
liability in Nevada in medical malpractice cases.
Statute of limitations-- Plaintiff must file within three years
from the injury or two years from the discovery of the
injury, whichever is first.
Bad faith claims-- The insurer we spoke to said it had not
faced many bad faith claims in Nevada.
Nevada
State specifics
Population: 1,998,257
Size (land area): 109,826 sq miles
Density: 18.2 pp/sq. mi
Premium Rates: General Surgery for Eight Nevada Insurers
($1M/$3M mature claims-made coverage)
Direct Losses Paid Compared to Direct Losses Incurred
Nevada 1975-2001
Direct losses paid
Direct losses incurred
Losses (in millions of 2001 dollars)
NV
Nevada Med. Liab. Co. (NML Ins. Co.) in South Region
P-I-E Mutual Ins. Co.in Clark County
Phys. Ins. Co. of Wisconsin (PlC Wisconsin) in Clark County
Michigan Physicians Mutual Liability Co. (MICOA) in Clark County
Medical Insurance Exchange of California (MIEC) in Clark County
Doctors' Company in Clark County
American Physicians Assurance Corp. (AP Capital) in Clark County
American Healthcare Indemnity Co. (SCPIE Cos.) in Clark County
Premium (dollars in thousands)
20
40
60
80
100
20022001200019991998199719961995199419931992
0
20
40
60
80
100
20011999199719951993199119891987198519831981197919771975
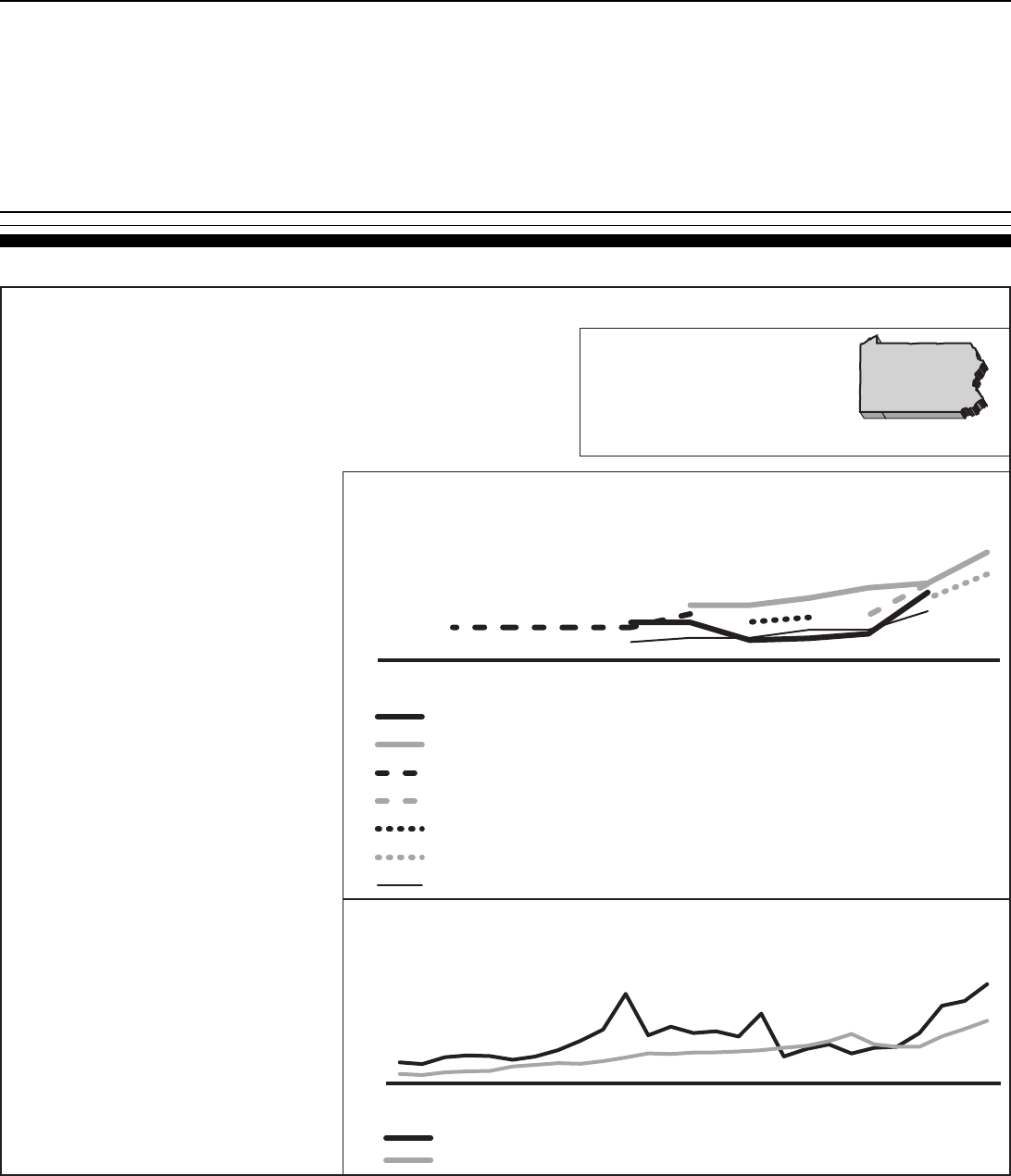
Appendix III
State Summaries
Page 64 GAO-03-702 Medical Malpractice Insurance
Figure 15: Pennsylvania
Sources: U.S. Census Bureau, 2000 (top box); GAO analysis of Medical Liability Monitor data (middle box); GAO analysis of A.M. Best data (bottom box).
Market description:
Typical coverage type and limit-- Until recently, insurers in Pennsylvania were still offering
occurrence coverage. By 2003, virtually all of the insurers in Pennsylvania will offer only claims-
made policies. PA requires $500,000 of private insurance; Mcare--the state sponsored patient
liability fund--will insure above this amount to $1.2 million.
Frequency and severity-- The Pennsylvania Insurance Department (PID) believes severity has
recently increased in PA. Both PID and Pennsylvania Medical Society Liability Insurance
Company (PMSLIC) believe this change in severity is responsible for increasing insurer losses.
Regional differences-- Most insurers charge higher rates for general surgery around Philadelphia.
Insurer characteristics and market share:
Insurer characteristics-- As of 2002, the largest
remaining medical malpractice insurer in the state is
PMSLIC, a physician-owned stock company. Other
entities writing in the state are commercial
companies, the state Joint Underwriting Association,
and self-insured academic health centers.
Market share-- Based on A.M. Best and NAIC data, the
companies with a 5% or more market share in
Pennsylvania (2001) were PMSLIC (19%), MIIX
Insurance Company (14%), Medical Protective
Company (8%), TriCentury Insurance Company
(6%), Lexington Insurance Company (5.2%), and
VHA Risk Retention Group Inc. (5.1%). Several large
medical malpractice insurersc--Phico, MIIX, and
Princeton--will have ceased writing in Pennsylvania
by the end of 2003.
Joint Underwriting Association-- The JUA covers around
5 hospitals and 1500 physicians and expects 1,000
more physicians to seek coverage in the next year.
Rate regulation:
The PID generally utilizes a file and use system with the
exception that it will review requests for more than a
10% increase in premium. PID only reviews small
commercial risks-those under $25,000 in premium-and
relies on the market to regulate large commercial risks.
State tort laws:
Limits on damage awards-- No limit on economic or
noneconomic damages.
Collateral source rule-- No modification.
Periodic award payments-- No specific provisions for
periodic award payments.
Pretrial expert certification-- Plaintiff's attorney must
sign the original complaint, certifying that the
attorney has contacted an expert who will attest to
the plaintiff's case.
Attorney contingency fees-- No modification.
Joint and several liability-- If the defendant is less than
60% responsible for the harm, defendant is liable for
only proportional share of ultimate judgment.
Statute of limitations-- Plaintiff must file within two years
of malpractice or discovery of injury.
Bad faith claims-- The insurer we spoke to said that this
was not a big issue in Pennsylvania.
Pennsylvania
State specifics
Population: 12,281,054
Size (land area): 44,817 sq miles
Density: 274 pp/sq. mi
Premium Rates: General Surgery for Seven Pennsylvania Insurers
(mature claims-made coverage–see market description for coverage limits)
Direct Losses Paid Compared to Direct Losses Incurred
Pennsylvania 1975-2001
Direct losses paid
Direct losses incurred
PA
Princeton Insurance Company
ProNational Ins. Co.in Philadelphia
Professionals Advocate in Philadelphia and Delaware Counties
Clarendon Nat. Ins. Co. in Delaware and Philadelphia County
P-I-E Mutual Ins. Co.in Delaware and Philadelphia Counties
Pennsylvania Medical Society Liability Insurance Co. (PMSLIC) in Philadelphia area
PHICO Insurance Co.in Delaware and Philadelphia Counties
Premium (dollars in thousands)
0
10
20
30
40
50
60
20022001200019991998199719961995199419931992
Losses (in millions of 2001 dollars)
0
100
200
300
400
500
20011999199719951993199119891987198519831981197919771975
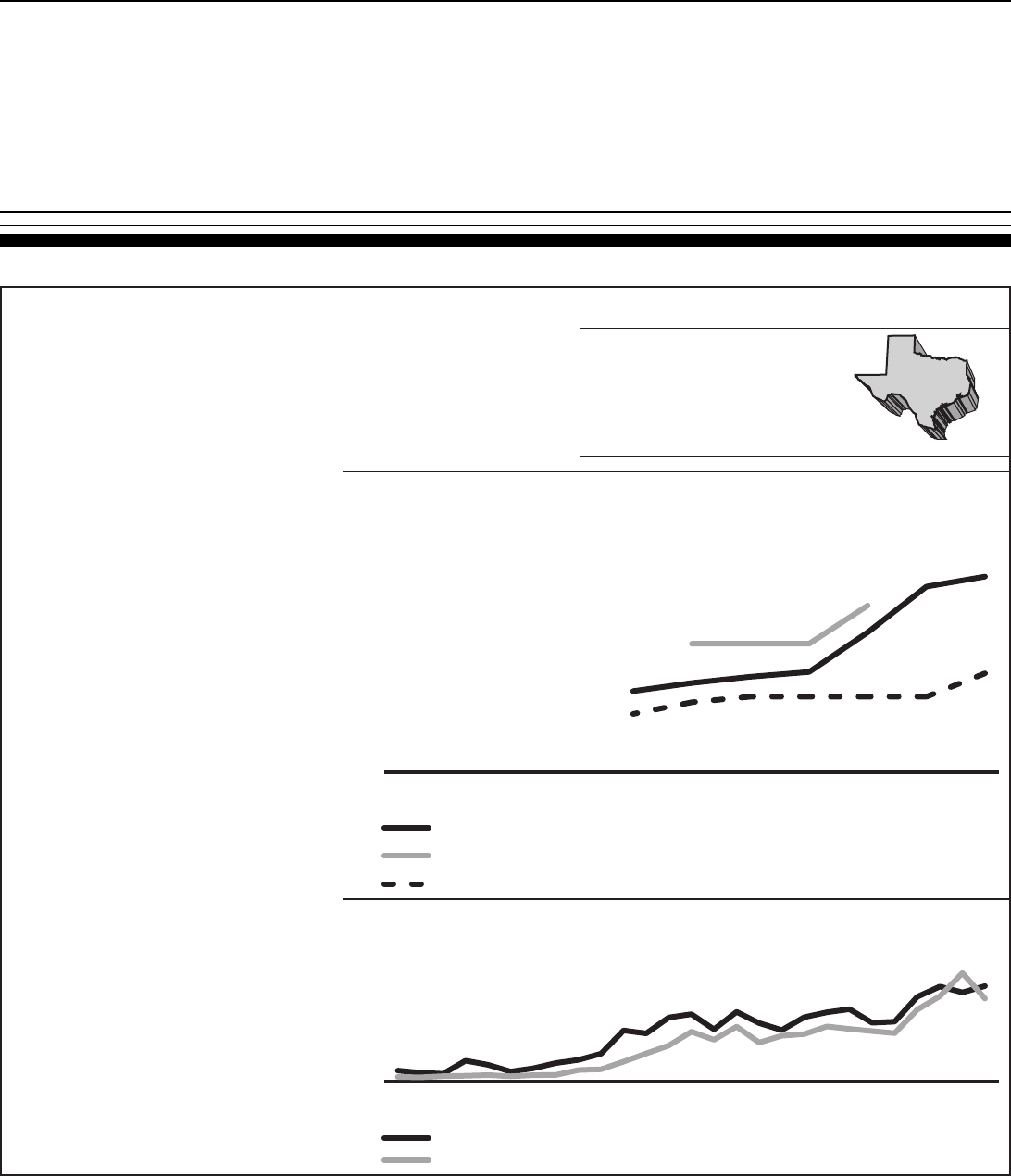
Appendix III
State Summaries
Page 65 GAO-03-702 Medical Malpractice Insurance
Figure 16: Texas
Sources: U.S. Census Bureau, 2000 (top box); GAO analysis of Medical Liability Monitor data (middle box); GAO analysis of A.M. Best data (bottom box).
Market description:
Typical coverage type and limit-- Majority of coverages written are claims made. Some physicians
have recently lowered their coverage limits; many now have $500,000 rather than the $1 million.
Frequency and severity-- A Texas Medical Association (TMA) study has shown frequency and
severity increasing in Texas. The Texas Department of Insurance (DOI) believes increases in
both severity and frequency have led to increased insurer losses.
Regional differences-- Most insurers reporting to the Medical Liability Monitor survey charge higher
rates for general surgery in urban areas such as Dallas and Houston, and the border county
El Paso.
Insurer characteristics and market share:
Insurer characteristics-- Licensed medical malpractice
insurance carriers cover one third of physicians,
unlicensed Texas Medical Liability Trust (TMLT)
covers one third, and one third are covered by
alternative forms of insurance.
Market share-- Based on A.M. Best and NAIC data, the
companies with a 5% or more market share in Texas
(2001) were TMLT (22%), Health Care Inemnity Inc.
(16%), and Medical Protective Company (10%). As of
2002 there were only four main writers of medical
malpractice insurance in Texas, down from 17 in
2001. Some went out of business, others
discontinued writing in Texas.
Joint Underwriting Association-- Formed in 1975, the
state JUA grew from 100 to 1,800 policies from the
late 1990s to January 2003.
Rate regulation:
Texas is a file and use state. In the mid 1990s, the state
mandated a rollback in premiums.
State tort laws:
Limits on damage awards-- Approximately $1.3 million
cap on noneconomic damages in wrongful death
cases. Texas applies the limit per plaintiff, per
defendant, and adjusts the limit for inflation.
Collateral source rule-- No modifications.
Periodic award payments-- No specific provision for
periodic award payments.
Pretrial expert certification-- Plaintiff must file either
cash, a cost bond, or an expert report within 90 days
of filing suit. Plaintiff must also serve expert report on
each defendant within 180 days of filing suit.
Attorney contingency fees-- No modification.
Joint and several liability-- Defendants can be liable for
payment of entire award if they are at least 51%
responsible for plaintiff's damages.
Statute of limitations-- Plaintiff must file the case within
two years of occurrence or discovery of the
malpractice.
Bad faith claims-- TMLT said bad faith claims are a
significant problem.
Texas
State specifics
Population: 20,851,820
Size (land area): 261,797 sq miles
Density: 79.6 pp/sq. mi
Premium Rates: General Surgery for Four Texas Insurers
($1M/$3M mature claims-made coverage)
Direct Losses Paid Compared to Direct Losses Incurred
Texas 1975-2001
Direct losses paid
Direct losses incurred
TX
Losses (in millions of 2001 dollars)
Medical Assurance in Dallas County
Amer Physicians Insurance Exchange in Hidalgo County
Texas Medical Liability Trust in El Paso County
Premium (dollars in thousands)
0
30
60
90
20022001200019991998199719961995199419931992
0
100
200
300
400
500
20011999199719951993199119891987198519831981197919771975
Page 66 GAO-03-702 Medical Malpractice Insurance
Appendix IV
GAO Contacts and Staff Acknowledgments Appendix IV
GAO Contacts
Richard J. Hillman, (202) 512-8678
Lawrence Cluff, (202) 512-8023
Acknowledgments
In addition to those individuals named above, Patrick Ward, Melvin
Thomas, Andrew Nelson, Heather Holsinger, Rudy Chatlos, Raymond
Wessmiller, Rachel DeMarcus, and Emily Chalmers made key contributions
to this report.
Page 67 GAO-03-702 Medical Malpractice Insurance
Related GAO Products
Medical Malpractice: Effects of Varying Laws in the District of Columbia,
Maryland, and Virginia. GAO/HEHS-00-5. Washington, D.C.: October 15,
1999.
Medical Malpractice: Federal Tort Claims Act Coverage Could Reduce
Health Centers' Costs. GAO/HEHS-97-57. Washington, D.C.: April 14, 1997.
Medical Liability: Impact on Hospital and Physician Costs Extends
Beyond Insurance. GAO/AIMD-95-169. Washington, D.C.: September 29,
1995.
Medical Malpractice Insurance Options. GAO/HEHS-94-105R.
Washington, D.C.: February 28, 1994.
Medical Malpractice: Maine's Use of Practice Guidelines to Reduce Costs.
GAO/HRD-94-8. Washington, D.C.: October 25, 1993.
Medical Malpractice: Estimated Savings and Costs of Federal Insurance
at Health Centers. GAO/HRD-93-130. Washington, D.C.: September 24,
1993.
Medical Malpractice: Medicare/Medicaid Beneficiaries Account for a
Relatively Small Percentage of Malpractice Losses. GAO/HRD-93-126.
Washington, D.C.: August 11, 1993.
Medical Malpractice: Experience with Efforts to Address Problems.
GAO/T-HRD-93-24. Washington, D.C.: May 20, 1993.
Practitioner Data Bank: Information on Small Medical Malpractice
Payments. GAO/IMTEC-92-56. Washington, D.C.: July 7, 1992.
Medical Malpractice: Alternatives to Litigation. GAO/HRD-92-28.
Washington, D.C.: January 10, 1992.
Medical Malpractice: Data on Claims Needed to Evaluate Health Centers'
Insurance Alternatives. GAO/HRD-91-98. Washington, D.C.: May 2, 1991.
Medical Malpractice: A Continuing Problem With Far-Reaching
Implications. GAO/T-HRD-90-24. Washington, D.C.: April 26, 1990.
(250093)
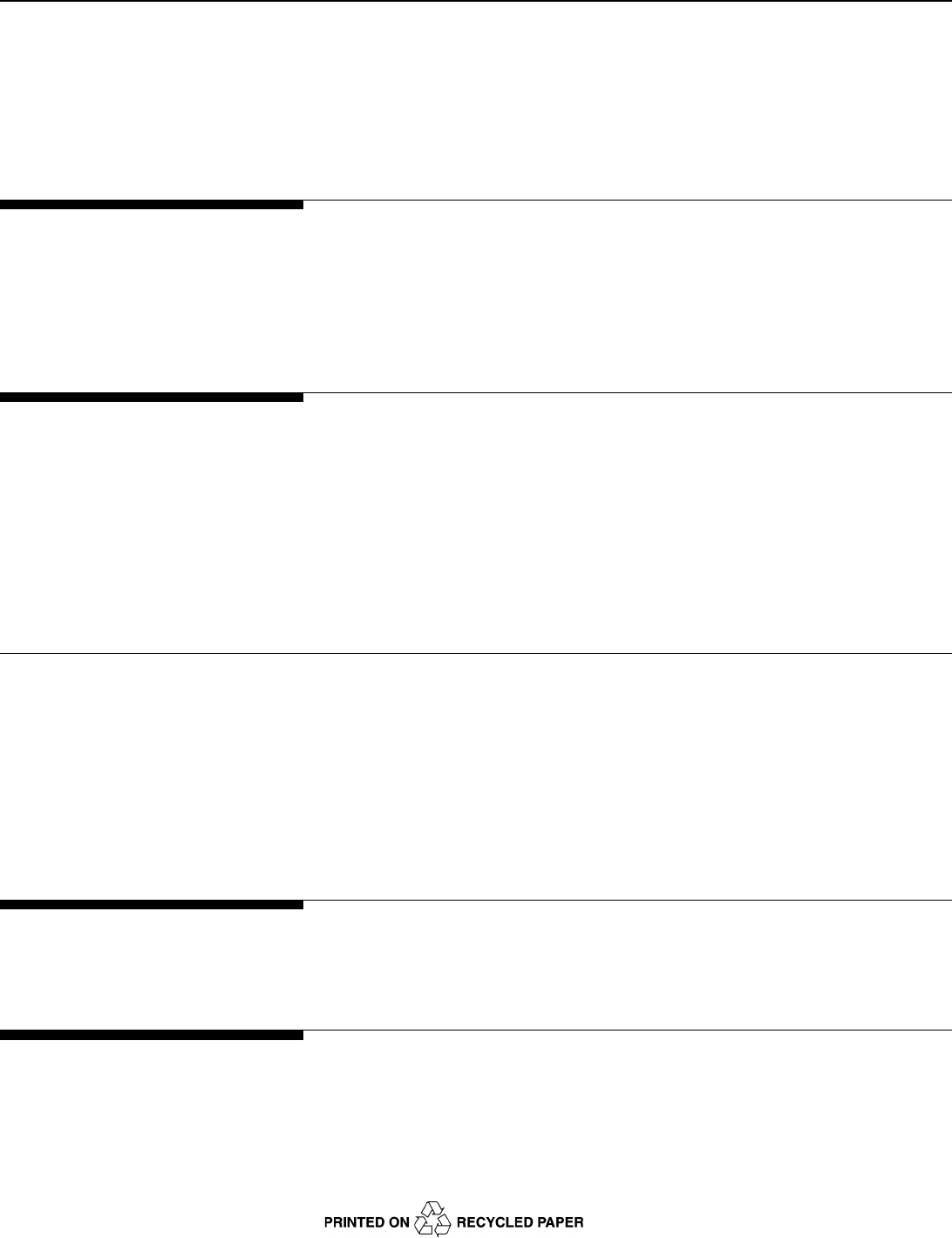
GAO’s Mission
The General Accounting Office, the audit, evaluation and investigative arm of
Congress, exists to support Congress in meeting its constitutional responsibilities
and to help improve the performance and accountability of the federal government
for the American people. GAO examines the use of public funds; evaluates federal
programs and policies; and provides analyses, recommendations, and other
assistance to help Congress make informed oversight, policy, and funding
decisions. GAO’s commitment to good government is reflected in its core values of
accountability, integrity, and reliability.
Obtaining Copies of
GAO Reports and
Testimony
The fastest and easiest way to obtain copies of GAO documents at no cost is
through the Internet. GAO’s Web site (www.gao.gov) contains abstracts and full-
text files of current reports and testimony and an expanding archive of older
products. The Web site features a search engine to help you locate documents
using key words and phrases. You can print these documents in their entirety,
including charts and other graphics.
Each day, GAO issues a list of newly released reports, testimony, and
correspondence. GAO posts this list, known as “Today’s Reports,” on its Web site
daily. The list contains links to the full-text document files. To have GAO e-mail this
list to you every afternoon, go to www.gao.gov and select “Subscribe to
e-mail alerts” under the “Order GAO Products” heading.
Order by Mail or Phone
The first copy of each printed report is free. Additional copies are $2 each. A check
or money order should be made out to the Superintendent of Documents. GAO
also accepts VISA and Mastercard. Orders for 100 or more copies mailed to a single
address are discounted 25 percent. Orders should be sent to:
U.S. General Accounting Office
441 G Street NW, Room LM
Washington, D.C. 20548
To order by Phone: Voice: (202) 512-6000
TDD: (202) 512-2537
Fax: (202) 512-6061
To Report Fraud,
Waste, and Abuse in
Federal Programs
Contact:
Web site: www.gao.gov/fraudnet/fraudnet.htm
E-mail: [email protected]
Automated answering system: (800) 424-5454 or (202) 512-7470
Public Affairs
Jeff Nelligan, Managing Director, [email protected] (202) 512-4800
U.S. General Accounting Office, 441 G Street NW, Room 7149
Washington, D.C. 20548


